Research Article
Genetic and Metabolic Diseases
JOURNAL
OF HEPATOLOGY
Alcohol consumption in late adolescence is
associated with an increased risk of severe liver
disease later in life
Graphical abstract
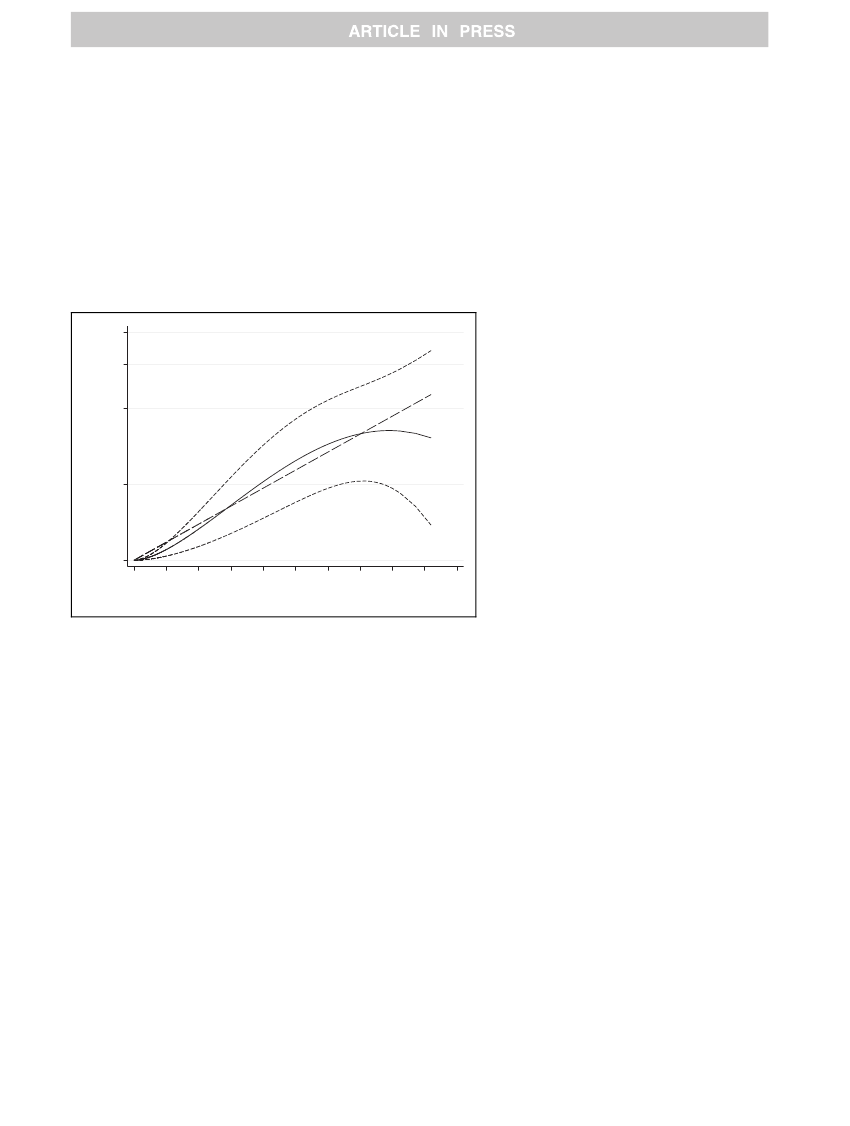
8.00
6.00
Authors
Hannes Hagström, Tomas Hemmingsson,
Andrea Discacciati, Anna Andreasson
Correspondence
4.00
Hazard ratio
(H. Hagström)
Lay summary
2.00
1.00
0
10
20
30
40
50
60
70
80
Alcohol consumption (grams per day)
90
100
Highlights
Alcohol consumption early in life was associated with an
increased risk for development of severe liver disease after
39 years of follow-up.
The risk increased in a dose-response pattern, with no
evidence of a threshold effect.
Trend towards an increased risk of severe liver disease in
men consuming less than current recommendations for a
safe alcohol intake.
We investigated more than 43,000 Swed-
ish men in their late teens enlisted for
conscription in 1969–1970. After almost
40 years of follow-up, we found that
alcohol consumption was a significant
risk factor for developing severe liver
disease, independent of confounders. This
risk was dose-dependent, and was most
pronounced in men consuming two
drinks per day or more.
http://dx.doi.org/10.1016/j.jhep.2017.11.019
Ó
2017 European Association for the Study of the Liver. Published by Elsevier B.V. All rights reserved. J. Hepatol. 2018, xxx, xxx–xxx