Tilsynet i henhold til grundlovens § 71 2012-13
§71 Alm.del Bilag 91
Offentligt
Deinstitutionalization and community basedservices in Italy –the experience in TriesteDr Roberto Mezzina, Director,WHOCC / MHDept., Trieste
0,212
0,4
0,6
0,8
1,2
1,4
1,6
1,8
0197519761977197819791980198119821983
1984198519861987198819891990
199119921993199419951996199719981999200020012002200320042005
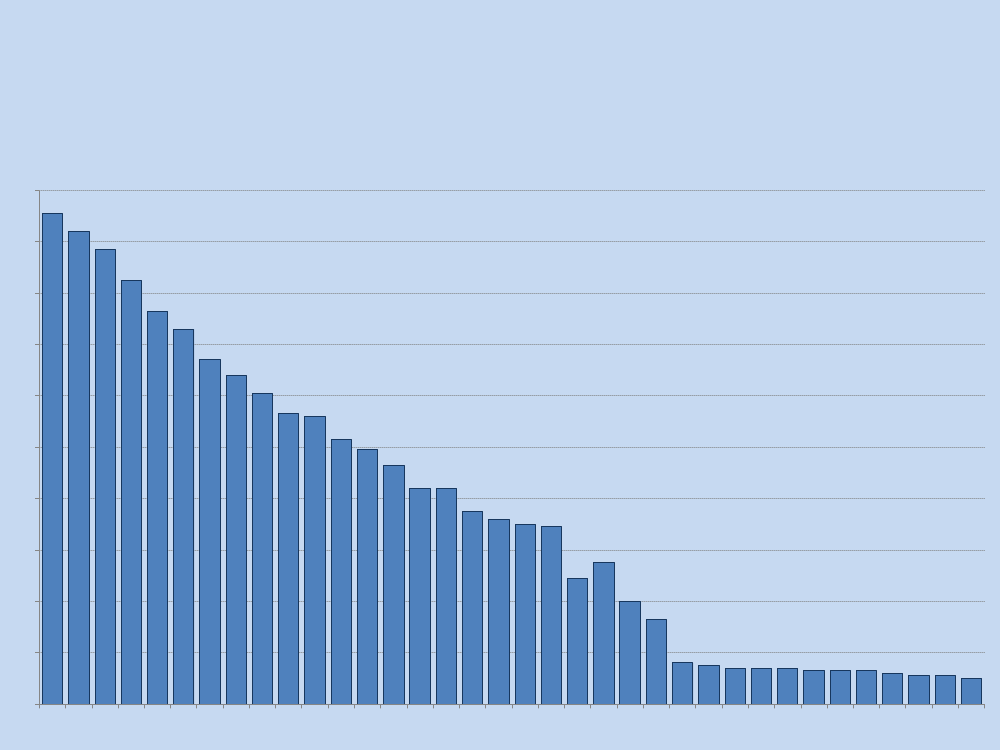
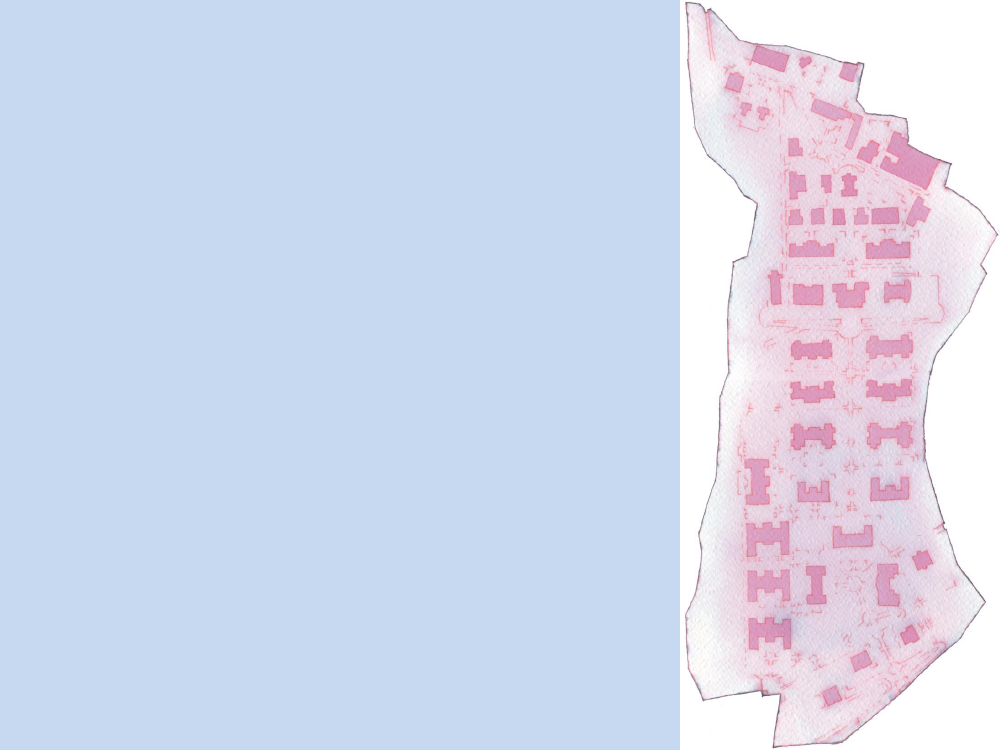
Number of psychiatric beds per 1 000population – Italy 1975-2010.Source: OECD health database
20062007200820092010
A picture of Italy today:13th of May 2013, 35 years later•100.000 inpatients in 1971 in PHs•48.000 inpatients in 1978•All PHs closed in 2000, 22 years after the1978Reform Law.IT DECLARED:-no Phs admission, no new PHs-community based care as a rule-human rights focus: involuntary treatmentduration reduced (1 week +) – 2 pych. to mayor-No police / justice involved – just health protection
Involuntary Treatment3 major conditions under which the IT could apply:•the person is affected by some kind of mental health illnessand subsequently needs urgent medical treatment;•the person refuses to be treated;•besides hospitalisation, there is no other timely andappropriate measure that could be undertaken to treat theperson.DATA•ITs accounted for50% of total admissions in 1975(3 yearsbefore the introduction of Law 180), whilst the figure droppedto 20% in 1984 and to approximately14% in recent years(DeGirolamo et al., 2006a).
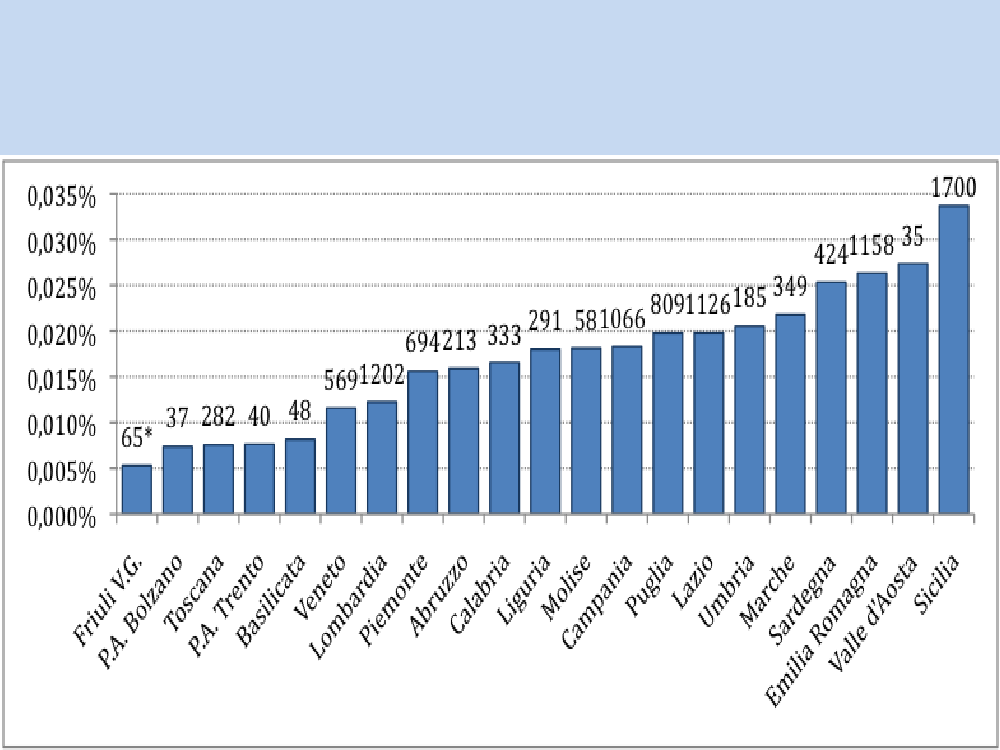
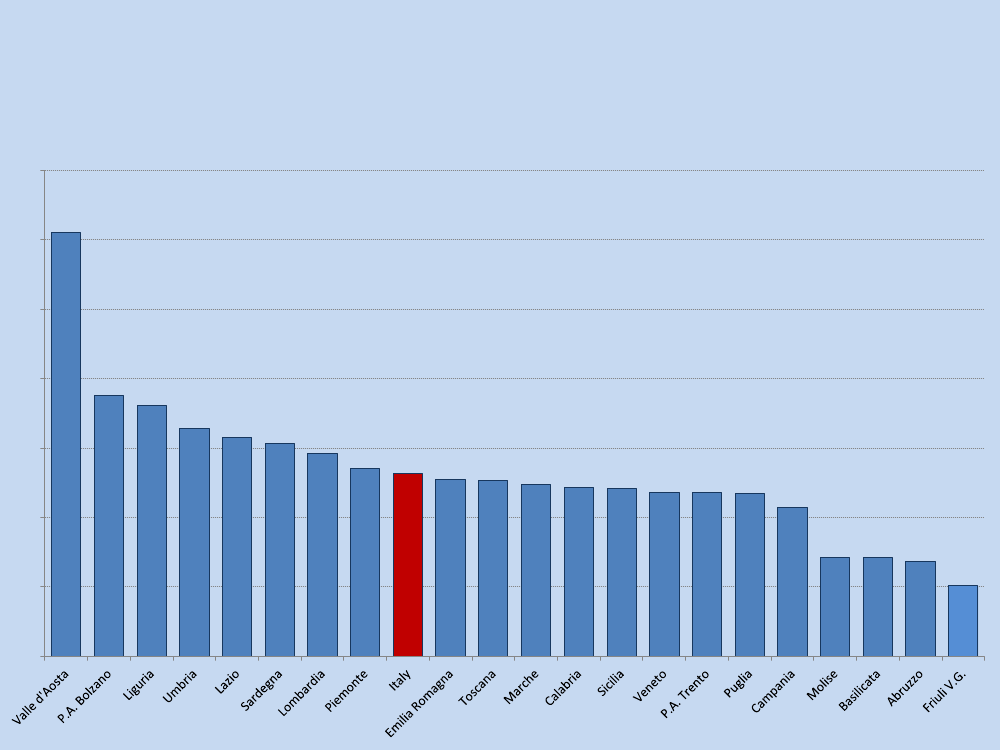
CTOs discharge rates out of total population and totalnumber of cases, by region – 2010Source: MINISTRY OF HEALTH
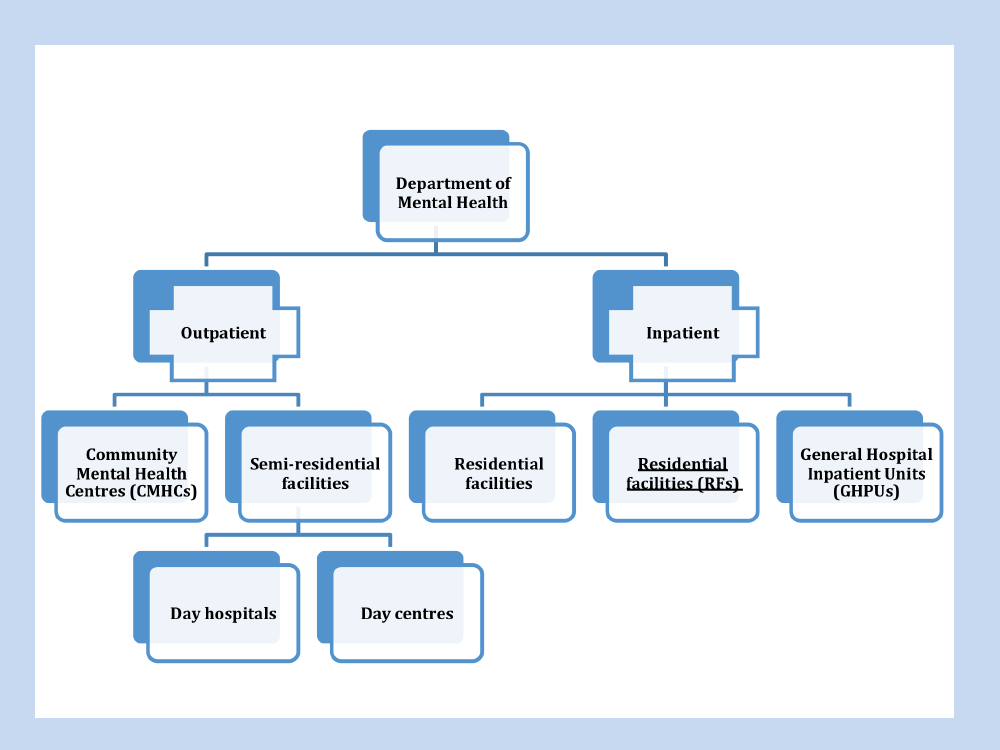
Mental Health Departments•They are rooted in areas of about 300.000inhabitants and encompasses a number ofcomponents:1. Small general hospital acute units (15 beds),1/10.0002. Community Mental Health Centers (up to 12hr,sometimes 24hr) 1/80.0003. Group-homes 2/10.000 with a wide range ofsupport up to 24hr (17.000 beds in Italy, mostlyNGOs)4. Day Centre (also with NGOs)
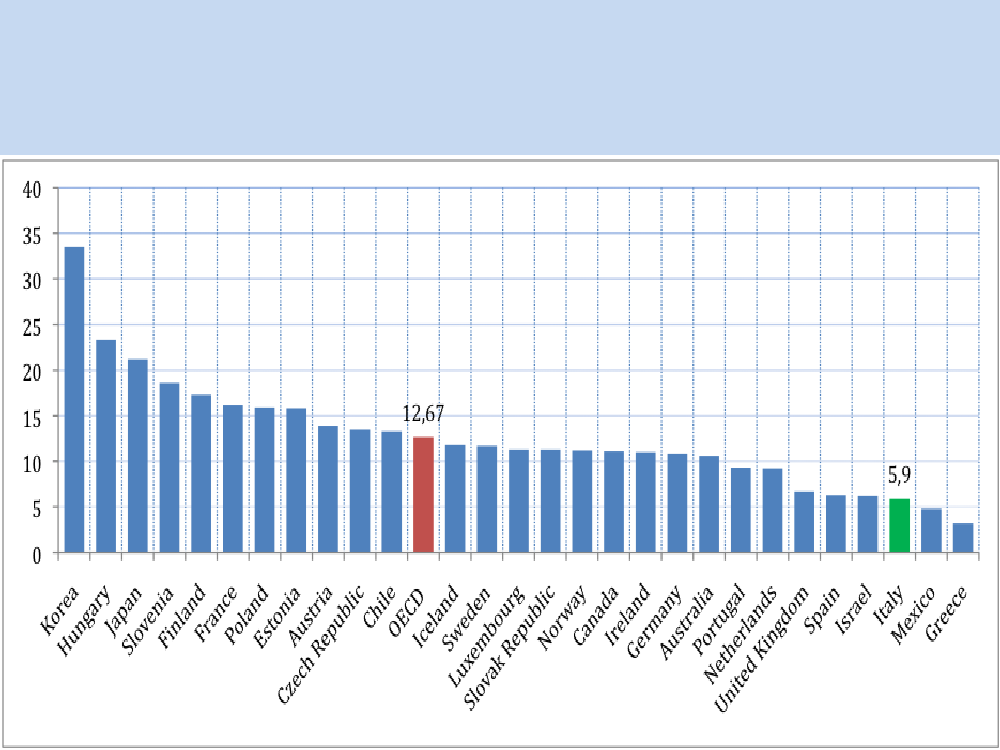
Italy and suicide•In 2010 there were 3 048 deaths for suicide in Italy,representing5.1 suicides per 100 000population(ISTAT, 2012).•One in threepeople who committed suicide during2010 was referred to be suffering from some kind ofmental health problem(1 100 cases) (ISTAT, 2012).•The suicide rate hasdecreased considerably from8.3per 100 000 population in 1993to 5.1per 100000 in 2010.
Suicide per 100 000 population in OECDcountries, 2010 or latest available year
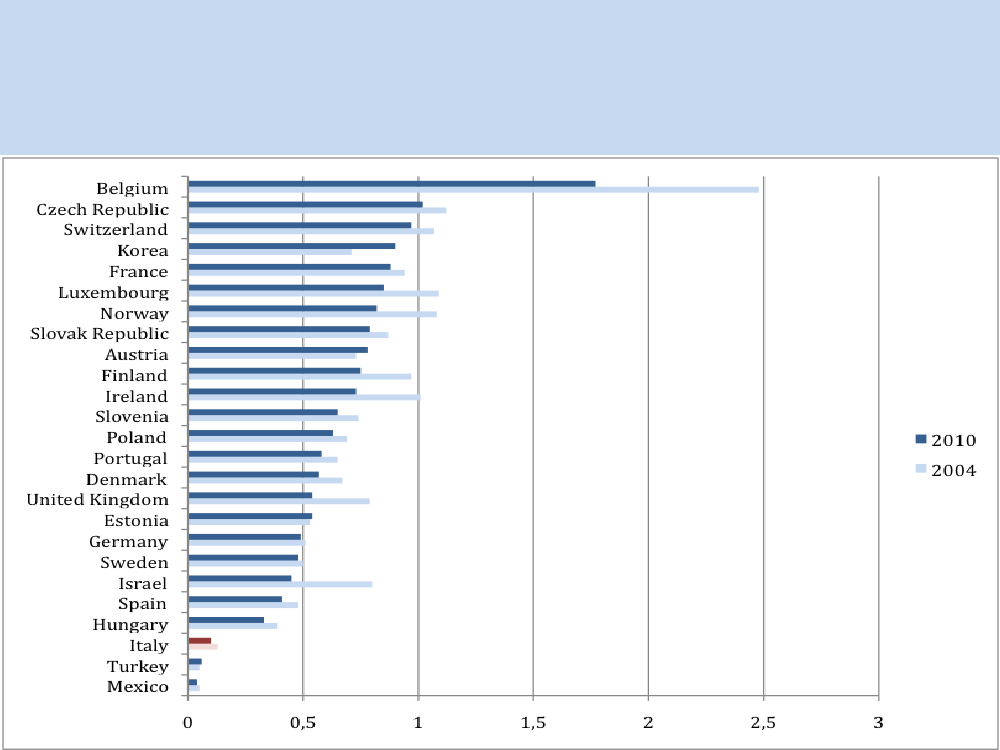
Psychiatric beds•With a rate of1.08 total psychiatric beds per 10 000inhabitants(over 18) (0.97 publicly and 0.11 privateaccredited beds), the availability of public acute bedsin Italy was slightly above the national standards in2009 (1 bed per 10 000 population).•Parallel to the increase of community-based mentalhealth services, the number of psychiatric beds inItaly hasdramatically decreasedover the last 35years, in line with the decrease in the overall numberof hospital beds (OECD health database 2013).
Psychiatric beds per 1 000 population in someOECD countries, 2004-2010.Source: OECD health database.
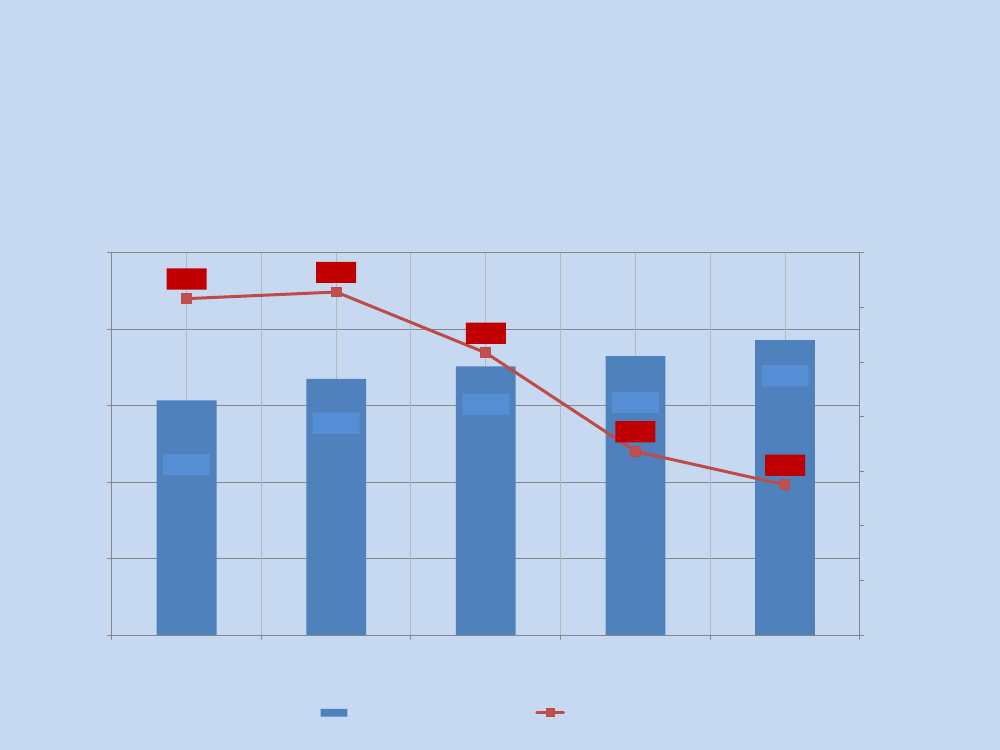
Unplanned schizophrenia re-admission rate (< 30 days fromdischarge - same hospital) out of total schizophrenia dischargesby region – 2010. SOURCE:MINISTRY OF HEALTH3530
25
20
15
13,15
10
5
0
Number of assistance days per user andpsychiatric beds provided in RFs, 2005-2009.SOURCE:MINISTRY OF HEALTH25.000221,6222,9220,020.000211,7210,015.000Beds16.76015.35110.00017.57618.259193,7187,5190,0Assistance days per user19.299200,0230,0
180,05.000
170,0
0
160,0
2005
2006
2007
2008
2009
Beds
Assistance days per user
Mental Health Care expenditure•As most of OECD countries, overall healthexpenditures in Italy have unevenly increased overthe last 10 years. The latest available data (2010)show that total health expenditures in Italyaccounted for above EUR 130 million (OECD healthdatabase 2013), which corresponds to approximately9% of GDP.This is in line with the average of OECDcountries.•It was established through the Conference of Regions(Conferenzadelle Regioni)thatno less than 5%ofthe local health budget would be allocated to mentalhealth services (WHO, 2011).
Changing public attitudeand family burden•Social acceptance of the law and a general decrease of stigmaattached to psychiatry mark a series of fundamental changesin public attitudes (DEMOskopea).•Cross-cultural researches demostrate this change incomparsion with other countries (Vicente et al 1995; Roelandtet al, 2007).•Other transnational researches demostrated less familyburden in the new community scenario (Fadden et al, 2002).•It is generally accepted that the Mental Hospitals belongs tothe past and cannot be accepted anymore.•Carers associations as UNASAM, as well as professional ones(e.g. the Society of Italian Psychiatrists), for many years claimfor better community services rather than for a new law.
Key lessons from Italy•A clear policy withinvestments•working directlywithin total institutions– not a simpleadminstrative closure•Totalreconversion of staff and resourcesof PH into community MHDepts (no parallel systems “hospital-community”, no doublespending);•creating alternativenetworks of coherent servicesthat work insynergy within the community, thereby•avoiding useless and oftenharmful fragmentationandspecialisations•Avoiding implementation of general hospital services only, insteadofcomprehenesive community mh centresand services.
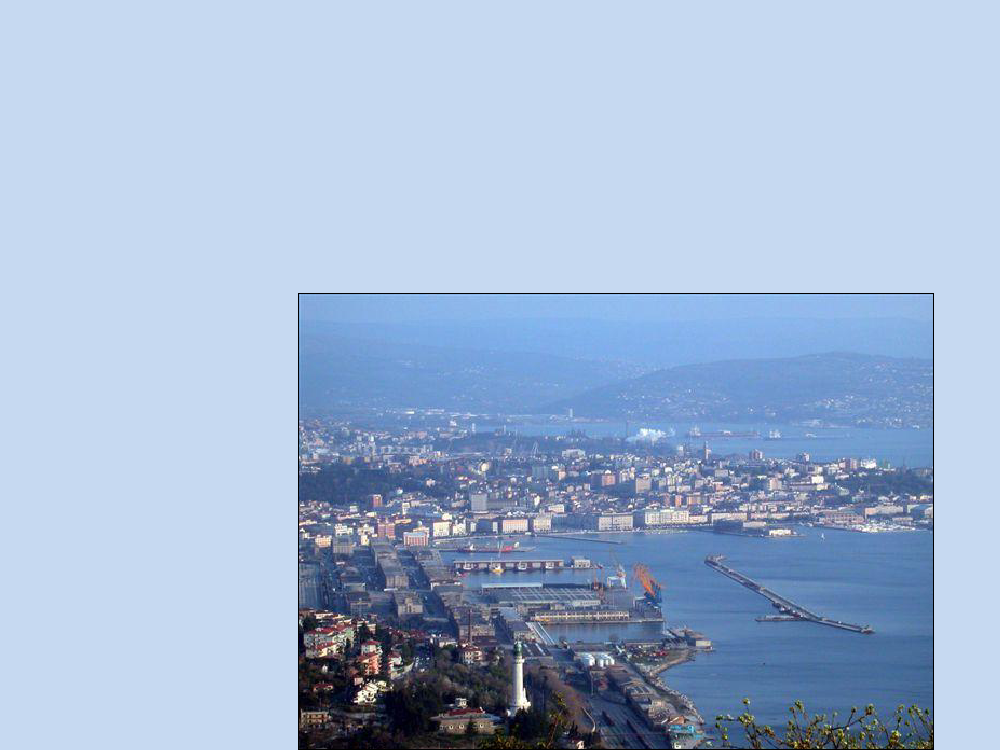
TRIESTE, the icon of the reform: a townwithout a psychiatrichospitalfor 35 years.From total institution to a fullycommunity based service,without barriers, immersed in the community, and a lowthreshold of access, with the highest degree offreedom,following the principle of aneed-based approachandnegotiation.
Today’s features in Trieste (WHO CC lead for servicedevelopment) are:Services:•4 Community Mental Health Centres(equipped with 6-8 beds each and openaround the clock) incl. the UniversityClinic•1 small Unit in the General Hospitalwith6 emergency beds;•Service for Rehabilitation andResidential Support(12 group-homeswith a total of 60 beds, provided by staffat different levels;•2 Day Centresincluding trainingprograms and workshops;•13accreditedSocial Co-operatives);•Families and users associations, clubsand recovery homes.Staff:•215 people- 1/1.000 (26 psychiatrists, 9psychologists, 130 nurses, 10 socialworkers, 6 psychosocial rehabilitationworkers).
Where are the ”beds” today?•Year 1971:•1200 bedsin PsychiatricHospital•Year 2012:•78 bedsof different kindin the community:•26 community crisis bedsavailable 24 hrs. MentalHealth Centres (11 /100.000 inhabitants)•6 acute bedsin GeneralHospital (3,5 / 100.000)•45 placesin group-homes(20 / 100.000)peppe dell'acqua dsm trieste whocollaborating center[email protected]19
What is aCMH Centre?Building an alchemy•Anopen door on the street•Amultidisciplinary teamin anormalised therapeutic environment(domestic)for day care and respite, socialisation and socialinclusion•Amultifunctional service:outpatient care, day care, night care forthe guests, social care & work, team base for home treatment andnetwork interventions, group & family meetings / therapies, teammeetings, mutual support, relatives and other lay people visits,inputs and burden relief.•Social cooperatives dohome management•Leisure anddaily life support(self care; brekfast, lunch and dinner)•And many other ordinary and straordinary things …
CSM DOMIO
CSMBARCOLA
•••••
•
Overarching criteria / principlesof community practice in the MH Dept.Responsibility (accountability) for the mental health of thecommunity = single point of entry and reference, publichealth perspectiveActive presence and mobility towards the demand = lowthreshold accessibility, proactive and assertive careTherapeutic continuity = no transitions in careResponding to crisis in the community = no acute inpatientcare in hospital bedsComprehensiveness = social and clinical care, integratedresourcesTeam work = multidisciplinarity and creativity in a wholeteam approach
Whole life approach = recovery and citizenship,person at the centre
A Value-driven Service
••••••
••••
Focus on a citizen with rightsHelping the person and not treating an illnessUnderstand events of life, overcome crisisExplain and discuss experienceNot losing value as a person (invalidation, neglect,violence)Keep social roles and maintaining social networks /systemsHelp social support networks e.g. familyDevelop growth potential (recovery)Have opportunities – real empowermentChange living conditions using material resources (work,money, practical help)
Some relevant outcomes•In 2010, only 16 persons underinvoluntary treatments (7 / 100.000inhabitants), the lowest in Italy(national ratio: 30 / 100.000); 2 / 3are done within the 24 hrs. CMHC;Open doors, no restraint, no ECT inevery place including hospital Unit;No psychiatric users are homeless;Social cooperatives employ 600disadvantaged persons, of which 30%suffered from a psychosis;Every year 240 trainees in SocialCoops and open employment, of which20-30 became employees;The suicide prevention programmelowered suicide ratio 50% in the last20 years (average measures);
••••
•
•
•
No patients in Forensic Hospitals.peppe dell'acqua dsm trieste whocollaborating center[email protected]24
How much does it cost?•1971:•Psychiatric Hospital5billions of Lire (today:28 million €)•2011:•Mental Health DepartmentNetwork18,0 millions €•79 € pro capita•94% of expenditures incommunity services, 6%in hospital acute bedspeppe dell'acqua dsm trieste whocollaborating center[email protected]25
Costs of MHD - 2010CostsStaffMedicationGeneral expenditure€ 11.158.171,01€ 1.077.500,03€ 2.920.853,95
%59%6%16%
Social expenditurePersonal HealthBudgetTotal
€
956.802,88
5%14%100%
€ 2.645.362,81€ 18.758.690,68
The coops: activities in Triestecleaningandbuildingmaintenance(diverseagencies)Canteens and catering, incl.Home service for elderlypeoplePorterage and transportLaundrytailoringInformaticarchivesforcouncils, etcfurniture and designcafeteria and restaurantservices (Teatro Verdi)Hotel TritoneFront-office and call-centerof public agencies
Museums’staffagricultural production andgardening handicraftcarpentryphoto, video and radioproductioncomputerservice,publishing trade, CD-Romserigraphicstheatreadministrative servicesGroup-homes (type A)ParkingBeach(Ausonia)
Personalised Plan (PP)PP funded by Personalised Healthcare Budget and organisedalong 3 axes indispensable for full social functioning andempowerment : housing, work, socialisation.The PP accesses other services (mental health services,healthcare districts, social services) and community resources(volunteers, social coops, associations, families), and works asmuch as possible within the user’s family, physical and socialsetting.The Healthcare Agency must guarantee the quality of the PP.
Personalised Plan (PP)identifies:
–needs/goals–expected results–interconnection of interventions–resources required–role/duties of professionals and services–verification (when & how)
ConclusionsThe transformation processrequiresmultiplelevels:•Involvement of civil society and of allstakeholders•Policy level•Legislation•Service models and practices•Inter-sectoral change (Mainstreaming of MHat community level, not in the GeneralHospitals only)
Key messages•The deinstitutionalisation process isnot only downsizing oreven suppressing psychiatric hospitals,but undertaking acomplex process of removing the ideology and power of theinstitution byputting the person over the institutionwiththeir subjectivity, needs, life story, significant relationships,social networks, social capital.•In order to do that, it is necessary toshift the powerin orderto empower people with mental health problems, shiftresources from hospitals to a range of community basedservices useful for his/her whole life. It opens pathways ofcare and programs that integrate social and health responsesand actions.
•This latter means no longer managingprocesses for exclusion through thesegregation of persons, but placing theindividual at the centre of the system, withtheir human and social rights, and their needs,in a perspective which isbased on theperson’s ‘whole life’ and on recovery fromthe experience of a mental disorder.
From hospitalisation to hospitalityInstitutional rulesInstitutionalised TimeInstitutionalised(ritualised) relations:among workers / and withusersTime of crisis disconnectedfrom ordinary lifeStay insideA stronger patients' roleMinimum network’s inputs•Agreed / flexible rules•Mediated time accordingto user’s needs•Relations tend to breakrituals•Continuity of carebefore/during/after thecrisis•Inside only for shelter/respite•Maximum co-presence ofSN
Hospitalisation / hospitalityDifficult to avoid:Locked doors•Isolation rooms•Restraint•ViolenceIllness /symptoms /body-brain•Open Door System
•Crisis / life events /experience / problems
The person and not the illnessat the center of theprocess of care for recovery and emancipationthrough users’ active participation in the services(up close, nobody is normal)