Sundhedsudvalget 2009-10
SUU Alm.del Bilag 517
Offentligt
World Alzheimer Report 2010The GlobAl economic impAcT of DemenTiA
World Alzheimer reporT 2010
Alzheimer’s Disease InternationalWorld Alzheimer Report 2010The Global Economic Impact of Dementiaprof Anders Wimo, Karolinska institutet, Stockholm, Swedenprof martin prince, institute of psychiatry, King’s College london, UKpublished by Alzheimer’s disease international (Adi) 21 September 2010
Acknowledgementsprofessor Bengt Winblad (Karolinska institutet, Stockholm, Sweden) and dr linusJönsson (i3 innovus and Karolinska institutet, Stockholm, Sweden) have contributedsignificantly to the methodological development in the cost estimates.Swedish Brain power (SBp) provided unrestricted financial support for the work ofAnders Wimo for this study.Alzheimer’s Association (US) for support with reviewing and launching this report.photos: Cathy Greenblat – www.cathygreenblat.comdesign: Julian howell
ADI would like to thank those who contributed financially:Vradenburg FoundationGeoffrey Beene Foundation – www.geoffreybeene.com/alzheimers.htmlAlzheimer’s Association – www.alz.orgAlzheimer’s Australia – www.alzheimers.org.auAlzheimer’s Australia WA – www.alzheimers.asn.auAlzheimer Scotland – www.alzscot.orgAlzheimer’s Society – www.alzheimers.org.ukAssociation Alzheimer Suisse – www.alz.chAlzheimerföreningen i Sverige – www.alzheimerforeningen.sedeutsche Alzheimer Gesellschaft – www.deutsche-alzheimer.deStichting Alzheimer Nederland – www.alzheimer-nederland.nl
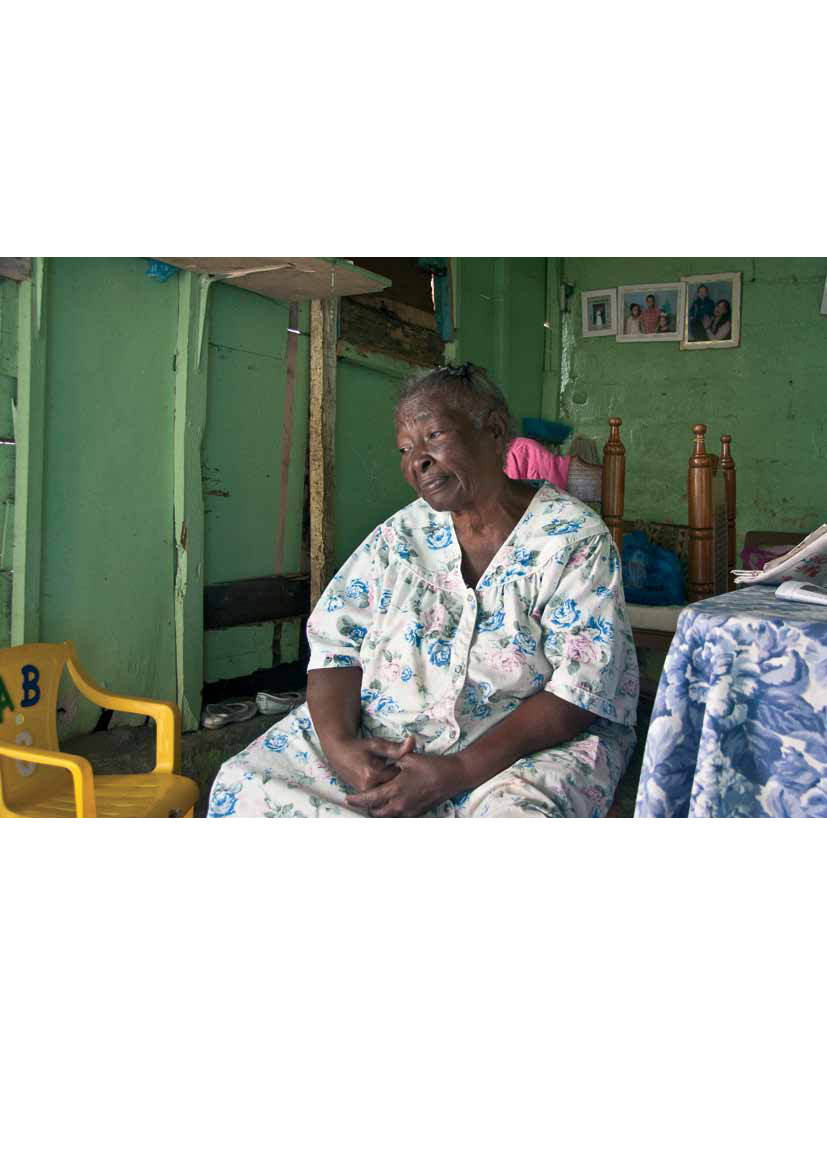
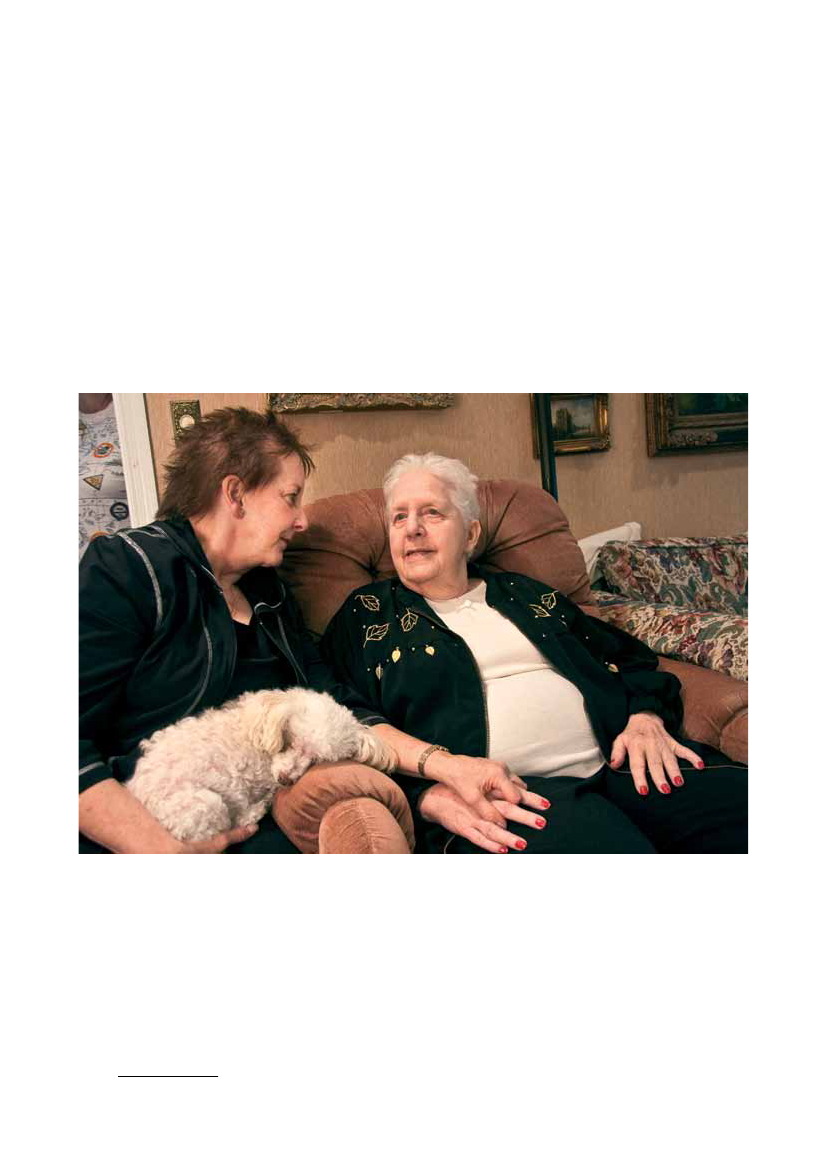
Cover imageAna de Jesus de Bido, a pastor and geriatrician, and her physicianhusband run a care facility in the Villa Francisca barrio in Santodomingo, dominican republic. here she was on a home visit with82-year-old Ana luisa Candelario, who cares for her 92-year-oldhusband. Ana luisa takes little care of herself, often not eating, andpastor Ana consoled her and explained the importance of caregiverstaking care of themselves.
The GloBAl eCoNomiC impACT oF demeNTiA
1
Alzheimer’s diseAse internAtionAl
World Alzheimer report 2010the GlobAl economic impAct of dementiA
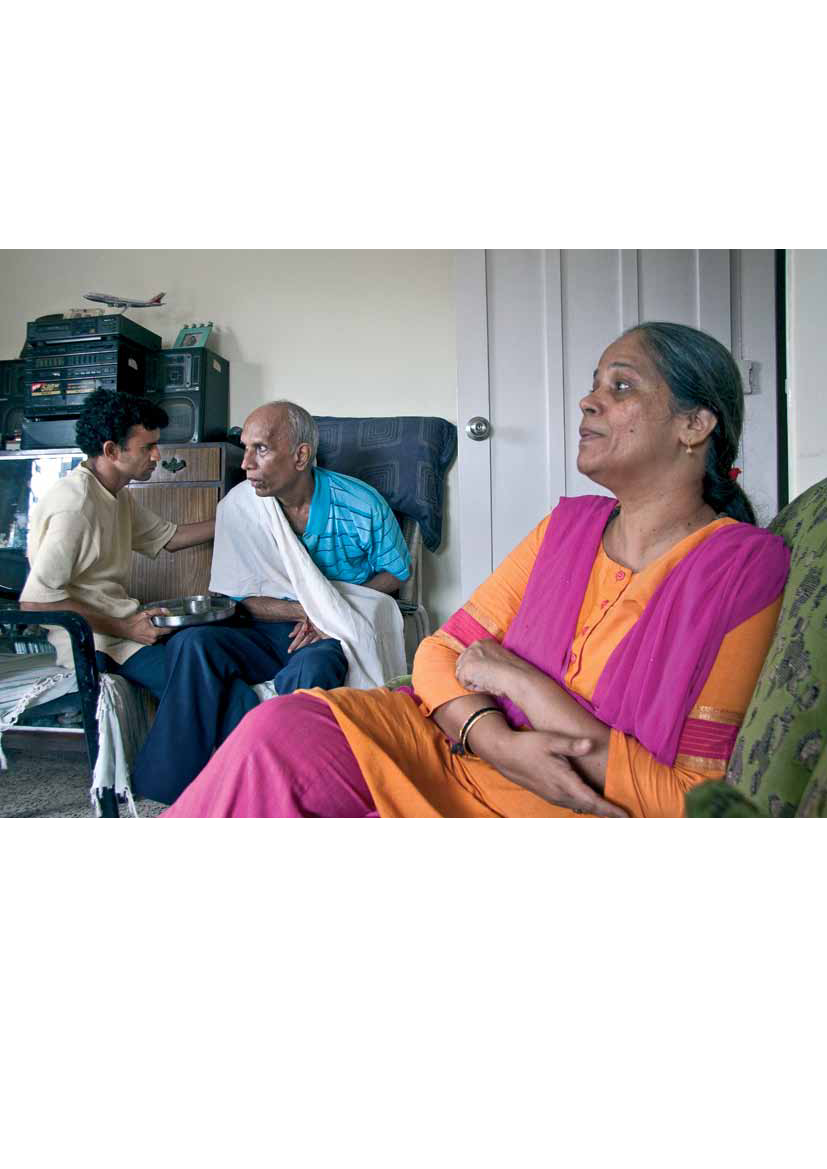
As mandakini became more confused, it was clear that she could no longer live alone. Two of her sons indicated thatthey could not take care of her because they had young children. her son Satish and his wife Neha, who also hadyoung children, brought her to their home, where they take care of her with the assistance of a professional caregiver.eight-year old Srushti has found ways to relate to her grandmother, and her two-year-old sister shows no fear. Thoughmandakini speaks very little, Srushti has found that her grandmother enjoys the religious chants that have beenimportant to her throughout her life. Now Srushti leads and they chant together.
2
World Alzheimer reporT 2010
forewordIn the World Alzheimer Report 2010, we build upon the findings detailed in the WorldAlzheimer Report 2009, to explore the cost of dementia to our societies. The Reportcontains an explanation of the methods used, detailed results for different economicand geographic regions, and we offer conclusions and recommendations in the finalsection.As you will see, the figures are cause for great concern and we hope that this Reportwill act as a call to action for governments and policy makers across the world. Itis vital that they recognize that the cost of dementia will continue to increase at analarming rate and we must work to improve care and support services, treatmentand research into dementia in all regions of the world. Lower income countries facea severe lack of recognition of dementia, placing a heavy burden on families andcarers who often have no understanding of what is happening to their loved one. Highincome countries are struggling to cope with the demand for services, leaving manypeople with dementia and caregivers with little or no support. Consequently, we urgekey decision makers to take notice of this very important document and to work withAlzheimer associations and with ADI to make dementia a national and global healthpriority.We would like to thank a number of people for their hard work on the developmentof this Report. We are grateful to the Report’s authors, Prof Anders Wimo and ProfMartin Prince, for their tireless efforts and dedication, and Niles Frantz and MaryKateWilson from the Alzheimer’s Association in the USA for their valuable input. Thankyou also to the sponsors who made the Report possible and to those who tookthe time to review the contents: the Organisation for Economic Co-operation andDevelopment (OECD) in Paris, the Alzheimer’s Association in the USA and GlennRees at Alzheimer’s Australia. Finally, we would like to thank Cathy Greenblat for herphotographs.Daisy AcostaChairmanAlzheimer’s disease international
Marc Wortmannexecutive directorAlzheimer’s disease international
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
3
contentsExecutive Summary 4Background4methods5results5Conclusions6recommendations7
Introduction 8previous evidence8references for introduction10
Methods 12Key design issues for cost of illness studies12prevalence versus incidence approaches12Top-down versus bottom-up approaches12Which costs are to be included, and how should they be computed?12The viewpoint13The representativeness of data sources on resource utilization13The ideal scenario for computing cost of illness … and the reality13Methods used in our cost of illness analyses14Summary14The evidence on the prevalence of dementia, and numbers affected worldwide14The evidence on the utilization of medical and social care, and informal care16
Results 24results of base option24Sensitivity analyses28how should we compare costs between countries, using a single cost metric?28Which informal care inputs should be included?29how should we cost the inputs of informal caregivers?30Comparison of this report with previous worldwide cost estimates of dementia32references for methods and results34
Conclusions and recommendations 38Strengths and weaknesses38The regional distribution of global costs39Comparisons with other estimates of the cost of dementia42Comparison with the cost of other chronic diseases44Alzheimer’s disease international’s recommendations45references for conclusions and recommendations48
Glossary 50Alzheimer’s Disease International 51
Alzheimer’S diSeASe iNTerNATioNAl
4
World Alzheimer reporT 2010
executive summaryThe total estimated worldwide costs of dementia are US$604 billion in 2010.About 70% of the costs occur in Western Europe and North America.Costs were attributed to informal care (unpaid care provided by family and others), directcosts of social care (provided by community care professionals, and in residential homesettings) and the direct costs of medical care (the costs of treating dementia and otherconditions in primary and secondary care).Costs of informal care and the direct costs of social care generally contribute similarproportions of total costs, while the direct medical costs are much lower. However, in lowand middle income countries informal care accounts for the majority of total costs anddirect social care costs are negligible.
Background• Dementia is a syndrome that can be caused by a number of progressive disorders that affectmemory, thinking, behaviour and the ability to perform everyday activities. Alzheimer’s diseaseis the most common type of dementia. Other types include vascular dementia, dementia withLewy bodies and frontotemporal dementia.• Dementia mainly affects older people, although there is a growing awareness of cases that startbefore the age of 65. After age 65, the likelihood of developing dementia roughly doubles everyfive years.• In last year’s World Alzheimer Report, Alzheimer’s Disease International estimated that there are35.6 million people living with dementia worldwide in 2010, increasing to 65.7 million by 2030and 115.4 million by 2050. Nearly two-thirds live in low and middle income countries, where thesharpest increases in numbers are set to occur.• People with dementia, their families and friends are affected on personal, emotional, financialand social levels. Lack of awareness is a global problem. A proper understanding of thesocietal costs of dementia, and how these impact upon families, health and social careservices and governments may help to address this problem.• The societal cost of dementia is already enormous. Dementia is already significantly affectingevery health and social care system in the world. The economic impact on families isinsufficiently appreciated.• In this World Alzheimer Report 2010, we merge the best available data and the most recentinsights regarding the worldwide economic cost of dementia. We highlight these economicimpacts by providing more detailed estimates than before, making use of recently availabledata that considerably strengthens the evidence base.– The World Alzheimer Report 2009 provides the most comprehensive, detailed and up-to-date data on the prevalence of dementia and the numbers of people affected in differentworld regions.– The 10/66 Dementia Research Group’s studies in Latin America, India and China haveprovided detailed information on informal care arrangements for people with dementia inthose regions.– For this Report, Alzheimer’s Disease International has conducted a global survey of keyinformants regarding the extent of use of care homes in different world regions.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
5
Methods• Different methods can be used to estimate the cost of an illness. The base approach in thisReport is a societal, prevalence-based gross cost of illness study. Annual costs per person withdementia for each country have been applied to the estimated number affected in that country,and then aggregated up to the level of World Health Organization regions, and World Bankincome groupings.• The costs considered include informal (family) care as well as direct medical and social carecosts. Direct medical costs refer to the medical care system, such as costs of hospital care,medication and visits to clinics. Direct social care costs are for formal services provided outsideof the medical care system, including community services such as home care, food supply andtransport, and residential or nursing home care.• For informal care, we estimated how much time family caregivers spend caring, includingtime spent with basic activities of daily living (such as eating, dressing, bathing, toileting andgrooming) and with instrumental activities of daily living (such as shopping, preparing food,using transport and managing personal finances).• The costs in this Report, as well as the prevalence of dementia, reflect estimates for 2010and are expressed as US dollars. To permit aggregation across countries, and comparisonsbetween countries and regions, costs were converted to US dollars from local currenciesbased on current exchange rates.• Cost of illness studies depend on a set of sources and assumptions. We have conductedcomprehensive sensitivity analyses in which we use different source data or vary assumptionsto see how this would affect the results (“Sensitivity analyses” on page 28).
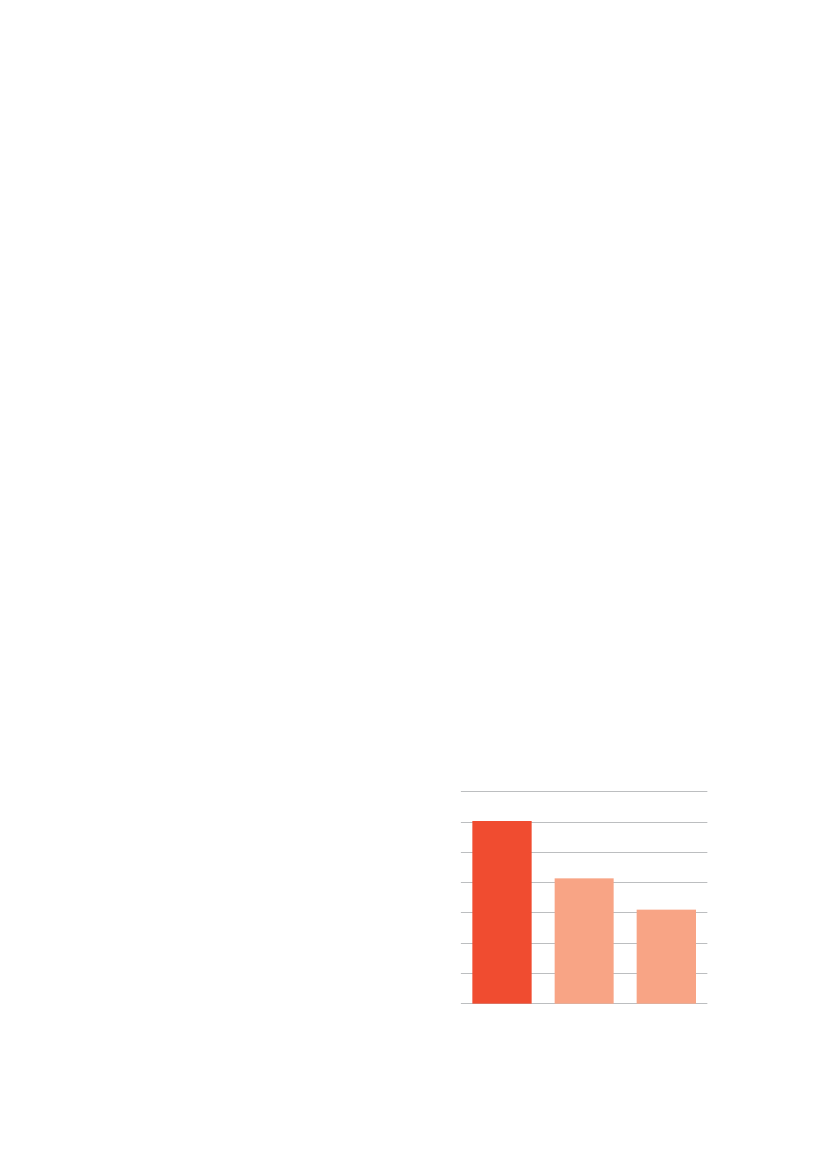
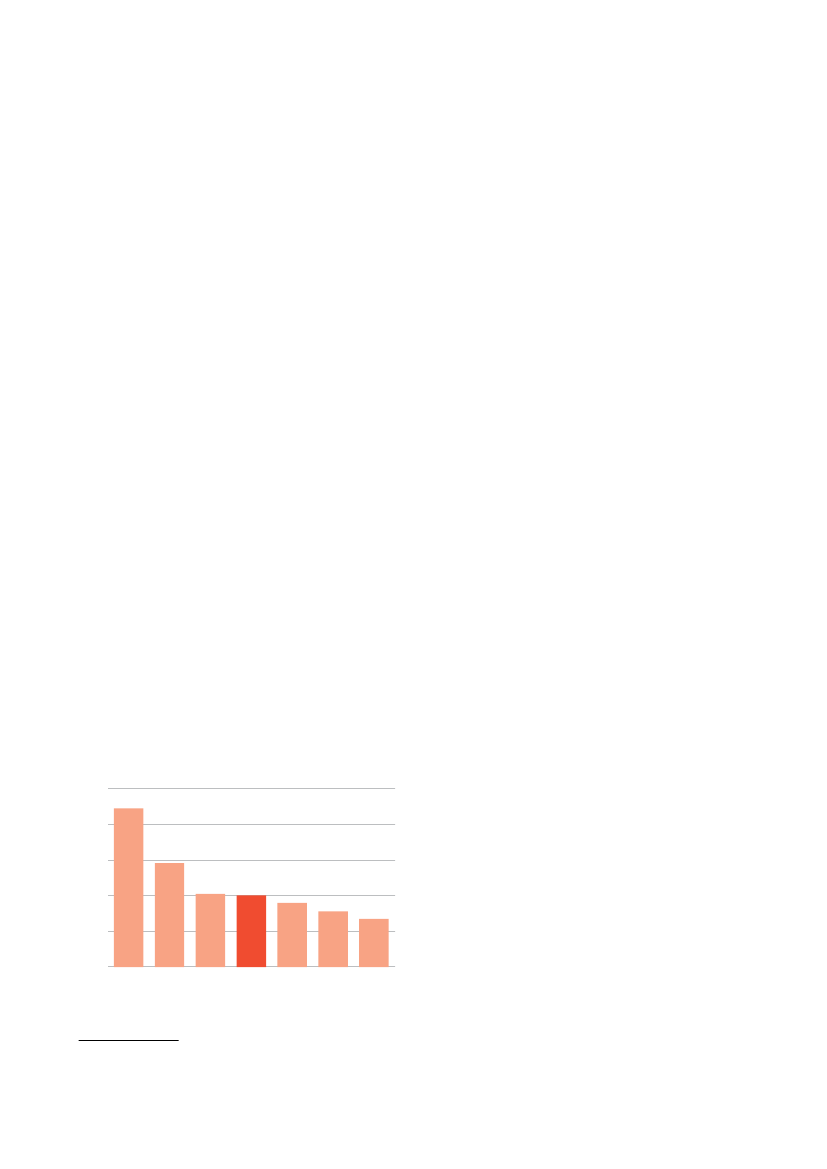
Results• The total estimated worldwide costs of dementia are US$604 billion in 2010.• These costs account for around 1% of the world’s gross domestic product, varying from0.24% in low income countries, to 0.35% in low middle income countries, 0.50% in high middleincome countries, and 1.24% in high income countries.• If dementia care were a country, it would bethe world’s 18th largest economy, rankingbetween Turkey and Indonesia. If it were acompany, it would be the world’s largest byannual revenue exceeding Wal-Mart (US$414billion) and Exxon Mobil (US$311 billion)(figure 1).• Costs of informal care (unpaid care providedby families and others) and the direct costsof social care (provided by community careprofessionals and in residential home settings)contribute similar proportions (42%) of totalcosts worldwide, while direct medical carecosts are much lower (16%).Figure 1Cost of dementia compared to companyrevenueUS$ billions700600500400300200100
• Low income countries accounted for just0DementiaWal-MartExxon Mobilunder 1% of total worldwide costs (but 14% ofthe prevalence), middle income countries forCost of dementia compared to company revenue10% of the costs (but 40% of the prevalence)and high income countries for 89% of the costs (but 46% of the prevalence). About 70% of theglobal costs occurred in just two regions: Western Europe and North America.
Alzheimer’S diSeASe iNTerNATioNAl
6
World Alzheimer reporT 2010
• These discrepancies are accounted for by the much lower costs per person in lower incomecountries – US$868 in low income countries, US$3,109 in lower middle income, US$6,827 inupper middle income and US$32,865 in high income countries.• In lower income countries, informal care costs predominate, accounting for 58% of all costsin low income and 65% of all costs in lower middle income countries, compared with 40% inhigh income countries. Conversely, in high income countries, the direct costs of social care(professional care in the community, and the costs of residential and nursing home care)account for the largest element of costs – nearly one half, compared with only one tenth inlower income countries.
Conclusions• The scale of the global cost of dementia is explainable when one considers that around 0.5% ofthe world’s total population live with dementia.– A high proportion of people with dementia need some care, ranging from support withinstrumental activities of daily living (such as cooking or shopping), to full personal care andround the clock supervision.– In some high income countries, between one third and one half of all people with dementialive in resource- and cost-intensive residential or nursing home care facilities.– Medical care costs also tend to be relatively high for people with dementia, particularly inhigh income countries with reasonable provision of specialist care services.• Costs are lower in developing countries, both per person and societally (as a proportion ofGDP). In these regions, there is a much greater reliance on the unpaid informal care provided byfamily and others.– While wage levels are low, these are increasing rapidly, and hence the opportunity cost orreplacement cost of these informal inputs is set to rise.– In our key informant survey, we estimated that in low and middle income countries only6% of people with dementia live in care homes. However, this sector is expanding rapidly,particularly in urban settings in middle income countries, boosted by demographic andsocial changes that reduce the availability of family members to provide care.– Medical help-seeking is relatively unusual in low and middle income countries, wheredementia is often viewed as a normal part of ageing. Demand for medical care is likelyto increase in the future, with improved awareness, better coverage of evidence-basedinterventions, and, possibly, more effective treatments.• Worldwide, the costs of dementia are set to soar. We have tentatively estimated an 85%increase in costs to 2030, based only on predicted increases in the numbers of people withdementia. Costs in low and middle income countries are likely to rise faster than in high incomecountries, because, with economic development, per person costs will tend to increasetowards levels seen in high income countries, and because increases in numbers of peoplewith dementia will be much sharper in those regions.• There is an urgent need to develop cost-effective packages of medical and social care thatmeet the needs of people with dementia and their caregivers across the course of the illness,and evidence-based prevention strategies. Only by investing now in research and cost-effectiveapproaches to care can future societal costs be anticipated and managed. Governments andhealth and social care systems need to be adequately prepared for the future, and must seekways now to improve the lives of people with dementia and their caregivers.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
7
Recommendations
123
Alzheimer’s Disease International calls on governments to make dementia a healthpriority and develop national plans to deal with the disease.Alzheimer’s Disease International reminds governments of their obligations underthe UN Convention on the Rights of People with Disabilities, and the MadridInternational Plan for Action on Ageing to ensure access to healthcare. It callson governments to fund and expand the implementation of the World HealthOrganization (WHO) Mental Health Gap Action Plan, including the packages of carefor dementia, as one of the seven core disorders identified in the plan.Alzheimer’s Disease International requests that new investment in chronic diseasecare should always include attention to dementia. For example, the WHO GlobalReport on ‘Innovative Care for Chronic Conditions’ alerts policymakers, particularlythose in low and middle income countries, to the implications of the decreases incommunicable diseases and the rapid ageing of populations. Healthcare is currentlyorganized around an acute, episodic model of care that no longer meets the needsof patients with chronic conditions. The WHO Innovative Care for Chronic Conditionsframework provides a basis on which to redesign health systems that are fit for theirpurpose.Alzheimer’s Disease International calls on governments and other major researchfunders to act now to increase dementia research funding, including research intoprevention, to a level more proportionate to the economic burden of the condition.Recently published data from the UK suggests that a 15-fold increase is required toreach parity with research into heart disease, and a 30-fold increase to achieve paritywith cancer research. International coordination of research is needed to make thebest use of resources.Alzheimer’s Disease International calls on governments worldwide to developpolicies and plans for long-term care that anticipate and address social anddemographic trends and have an explicit focus on supporting family caregivers andensuring social protection of vulnerable people with dementia.Alzheimer’s Disease International supports HelpAge International’s call forgovernments to introduce universal non-contributory social pension schemesi.Alzheimer’s Disease International calls on governments to ensure that people withdementia are eligible to receive and do receive disability benefits, where suchschemes are in operation.
4
567
i http://www.helpage.org/Researchandpolicy/Socialprotection
Alzheimer’S diSeASe iNTerNATioNAl
8
World Alzheimer reporT 2010
introductionAlzheimer’s Disease International’s first WorldAlzheimer Report, released on 21 September 2009,provided up-to-date information on the prevalenceand impact of dementia from a global perspective(1).We estimated 35.6 million people living withAlzheimer’s disease and other dementias worldwidein 2010, increasing to 65.7 million by 2030 and 115.4million by 2050. We highlighted that nearly two-thirdsof all people with dementia lived in low and middleincome countries, this proportion being set to growbecause the sharpest increases in the numbers ofpeople with dementia will be in rapidly developingregions including Latin America, China and India.People with dementia, their families and friends areaffected on personal, emotional, financial and sociallevels. In the 2009 Report, we advocated for greaterawareness, more services, more funding for researchand, ideally, national dementia strategies in everycountry worldwide(1).In this World Alzheimer Report 2010, we focus onthe economic impact of dementia, again providingthe latest and most reliable estimates possible fromthe available evidence. Lack of awareness is a globalproblem, leading to common misunderstandingsabout Alzheimer’s disease and other forms ofdementia:• It is not a very common problem.• It is a normal part of ageing.• Nothing can be done.• Families will provide care – it is not an issue forhealth care systems or for governments.A proper understanding of the societal costs ofdementia, and how these impact upon families,health and social care services and governmentsmay help to correct these misapprehensions.Dementia is already significantly affecting everyhealth system in the world, and large amounts ofmoney are spent in caring for people with dementia.The aim of this Report is to highlight these economicimpacts so that governments, health and social caresystems are adequately prepared for the future, andcan seek ways to improve the lives of people withdementia and their caregivers now.Cost of illness (CoI) studies are descriptive. Theycan be used to quantify the total societal economicburden of a health condition, and can highlight therelative impact on different health and social caresectors. The distribution of costs between differentcountries and regions can also be estimated and
What is dementia?dementia is a syndrome that can be caused bya number of progressive illnesses that affectmemory, thinking, behaviour and the ability toperform everyday activities. alzheimer’s diseaseis the most common type of dementia. Othertypes include vascular dementia, dementia withLewy bodies and frontotemporal dementia. theboundaries between the types are not clear, anda mixture of more than one type is common.dementia mainly affects older people, althoughthere is a growing awareness of cases that startbefore the age of 65. after age 65, the likelihoodof developing dementia roughly doubles everyfive years. a detailed overview of dementia canbe found in the World alzheimer Report 2009,available from www.alz.co.uk/worldreport.
compared. CoI studies can also be used to describeor (with less certainty) predict changes in the extentor distribution of costs over time. While CoI studiesconducted on different health conditions can beused to compare burden, some caution is needed inusing these estimates to set priorities. The methodsused, particularly the types of costs included orexcluded, and the data used to estimate them maynot be strictly comparable across different healthconditions. Also, it has been argued that prioritizationfor investment in healthcare should be determinedby the relative incremental cost-effectiveness ofavailable interventions, rather than the burden of thedisease(2). Transparency is crucial with regard to theassumptions underlying any cost calculations andcomparisons.
Previous evidenceCost of illness studies for dementia have alreadybeen carried out for some regions and countries,mainly from high income parts of the world: forexample, Europe(3), United Kingdom(4), Sweden(5),Australia(6), the USA(7)and Canada(8). All thesereports have shown that Alzheimer’s and otherdementias are imposing huge societal economicburdens, both through direct (medical and socialcare) and indirect (unpaid caregiving by families andfriends) costs. Evidence is just beginning to emergeof the extent of the economic burden in middleincome countries(9-12).
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
9
Previously, three papers that highlight the globaleconomic burden have been published(13-15). Thesereports were, at the time of their publication, basedon the best available data for Alzheimer’s anddementia. Cost estimates were generated fromthe Dementia Worldwide Cost Database (DWCD) acontinuously updated resource maintained at theKarolinska Institutet Alzheimer’s Research Center,Stockholm, Sweden. The most recent of thesethree reports updated previous estimates of globalcosts from US$315 billion in 2005 to US$422 billionin 2009, an increase of 34% (18% in fixed prices)in just four years(15). US$312 billion per year (74%of the worldwide total) is contributed by countriesdesignated by the UN as more developed regionsand 110 billion (26% of the total) by less developedregions.One major limitation of these papers was that theDWCD contained very few data from low and middleincome countries and Eastern Europe. Therefore,the cost models relied largely on extrapolation ofeconomic conditions from higher to lower incomecountries, adjusted for Gross Domestic Product(GDP) per person. Also, it was not possible todistinguish between direct medical costs (withinthe health care sector) and direct social care costs(within the community and care home sector). Whilewe still have incomplete data, the evidence-base hasbeen strengthened in three respects:
1 The World Alzheimer Report 2009 provides themost comprehensive, detailed and up-to-datedata on the prevalence of dementia and thenumbers of people affected in different worldregions(1).2 The 10/66 Dementia Research Group’sstudies in Latin America, India and China haveprovided detailed information on informal carearrangements for people with dementia in thoseregions(1,16).3 Alzheimer’s Disease International has conducteda global survey of key informant opinionsregarding the extent of use of care homes indifferent world regions.In this Report, we are merging the best available dataand the most recent insights regarding the worldwidecost of Alzheimer’s and other dementias. Clearly,the societal cost of dementia is already enormous.With the forecast growth in disease prevalence(1),costs will rise further, particularly in low and middleincome countries. There is an urgent need to developcost-effective packages of medical and social carethat meet the needs of people with dementia andtheir caregivers across the course of the illness,and evidence-based prevention strategies. Onlyby investing now in research and cost-effectiveapproaches to care can future societal costs beanticipated and managed.
When a caregiver in a Kyoto grouphome embraced this residenteveryone around smiled. Althoughit is widely held that touching is notappropriate in Japanese culture,dr Yoshio miyake explained that‘in Japan, training courses forprofessional caregivers of peoplewith dementia take place in manyand different settings, where non-verbal communication with them,including touch or physical contact, isemphasised very often.’
Alzheimer’S diSeASe iNTerNATioNAl
10
World Alzheimer reporT 2010
references for introduction(1) Alzheimer’s Disease International. World Alzheimer Report2009. London: Alzheimer’s Disease International; 2009.(2) Williams A. Calculating the global burden of disease:time for a strategic reappraisal? Health Econ 1999February;8(1):1-8.(3) Wimo A, Jönsson L, Gustavsson A, McDaid D, Ersek K,Georges J. The economic impact of dementia in Europein 2008 – cost estimates from the Eurocode project.International Journal of Geriatric Psychiatry. In press 2010.(4) Knapp, M. and Prince M. Dementia UK – A report into theprevalence and cost of dementia prepared by the PersonalSocial Services Research Unit (PSSRU) at the LondonSchool of Economics and the Institute of Psychiatry atKing’s College London, for the Alzheimer’s Society. THEFULL REPORT. London: The Alzheimer’s Society; 2007.(5) Wimo, A., Johansson, L., and Jönsson, L.Demenssjukdomarnas samhällskostnader och antaletdementa i Sverige 2005 (The societal costs of dementiaand the number of demented in Sweden 2005) (inSwedish). Stockholm: Socialstyrelsen; 2007. Report No.:2007-123-32.(6) Access Economics PTY Limited. The Dementia Epidemic:Economic Impact and positive solutions for Australia.Canberra: Access Economics PTY Limited; 2003.(7) US Alzheimer’s Association. 2010 Alzheimer’sdisease facts and figures. Alzheimers Dement 2010March;6(2):158-94.(8) Alzheimer Society of Canada. Rising Tide: The Impact ofDementia on Canadian Society. A study commissioned bythe Alzheimer Society. Toronto, Ontario: Alzheimer Societyof Canada; 2010.(9) Wang H, Gao T, Wimo A, Yu X. Caregiver time and costof home care for Alzheimer’s disease: a clinic-basedobservational study in Beijing, China. Ageing Int. In press2010.(10) Wang G, Cheng Q, Zhang S, Bai L, Zeng J, Cui PJ et al.Economic impact of dementia in developing countries: anevaluation of Alzheimer-type dementia in Shanghai, China.J Alzheimers Dis 2008 September;15(1):109-15.(11) Allegri RF, Butman J, Arizaga RL, Machnicki G, SerranoC, Taragano FE et al. Economic impact of dementia indeveloping countries: an evaluation of costs of Alzheimer-type dementia in Argentina. Int Psychogeriatr 2007August;19(4):705-18.(12) Zencir M, Kuzu N, Beser NG, Ergin A, Catak B, SahinerT. Cost of Alzheimer’s disease in a developing countrysetting. Int J Geriatr Psychiatry 2005 July;20(7):616-22.(13) Wimo A, Jönsson L, Winblad B. An estimate of theworldwide prevalence and direct costs of dementia in2003. Dement Geriatr Cogn Disord 2006;21(3):175-81.(14) Wimo A, Winblad B, Jönsson L. An estimate of the totalworldwide societal costs of dementia in 2005. Alzheimer’sand Dementia 2007;(3):81-91.(15) Wimo A, Winblad B, Jönsson L. The worldwide societalcosts of dementia: Estimates for 2009. Alzheimers Dement2010 March;6(2):98-103.(16) Prince M, Ferri CP, Acosta D, Albanese E, Arizaga R,Dewey M et al. The protocols for the 10/66 DementiaResearch Group population-based research programme.BMC Public Health 2007 July;7(1):165.
Alzheimer’S diSeASe iNTerNATioNAl
11
methods
World Alzheimer report 2010
Ten years ago, when Vijay was 52, he and Anu were told thathis increasing problems were due to early onset Alzheimer’s.They were not prepared for this news, but Anu managed thefamily life and become the sole earner. She pursued manyavenues to find what Vijay needed. Anu also sought out andbenefited from advice and assistance from others and shejoined a support group. She loves Vijay very much and benefitsfrom the assistance of mr deepak, a caregiver seen herefeeding Vijay. Anu now offers support and advice to othercaregivers through ArdSi and she willingly shares her storythrough the mass media to create better understanding andfight stigma.
Alzheimer’S diSeASe iNTerNATioNAl
12
World Alzheimer reporT 2010
methodsKey design issues for cost of illness studiesPrevalence versus incidenceapproachesCoI studies can either be prevalence or incidencebased. With the prevalence approach, the averagecosts are computed from all people in a populationfound to be affected at a specified time, with datacollected in a cross-sectional survey; peoplewith dementia will include some recently incidentcases, and others at varying stages in the diseasecourse(1,2). The rate at which the costs are observedto occur are then applied to a given period, typicallyone year, to compute the annual cost of illness,either as an average for each person with dementiaor, by multiplying by the total numbers affected, fora whole country or region. An alternative approachis to use longitudinal data (in which people withassumed newly diagnosed dementia (incident cases)have been followed up over time) to estimate thetypical costs of illness over the disease course,as annual costs and the future (discounted) costsduring the expected or calculated survival period.This approach can also be applied, although lessaccurately, to cross-sectional data. The choice ofapproach depends on the purpose of the study; ifthe idea is to estimate the aggregated economicsocietal burden of a condition for a country or region,the prevalence approach is suitable. If the aim is toillustrate the economic consequences of evolvingand cumulative care needs within individuals overtime, then the longitudinal approach is preferable.in Latin America, India and China demonstrate thatfor older people, at the population level, dementiais overwhelmingly the leading contributor amongchronic diseases to disability(3)and needs forcare(4). It was also demonstrated that for peoplewith dementia, it was the severity of dementia (asopposed to comorbid stroke, number of physicalimpairments or depression) that was the majorcontributor to hours of ADL care(5). However, the‘net’ costs of healthcare (costs that only depend ondementia as opposed to other comorbid conditions)are often difficult to estimate.
Which costs are to be included, andhow should they be computed?Care resources are generally scarce, so the use ofa resource in one way will result in a loss of benefitssomewhere else(6). Opportunity cost is the value ofa resource in its best alternative use(7), and this isthe approach recommended by most economists.Ideally, opportunity costs are based on marketprices. However, with respect to care, market pricesare not easy to identify and collect.Costs of illness are often sub-classified as directmedical costs, direct social care costs and indirectcosts. Direct cost calculations are typically based onthe value of resources used while indirect costs arebased on resources lost.Direct medical costsrefer to the medical caresystem, such as costs of hospital care, drugs andvisits to clinics.Direct social care costsarise from formal servicesprovided outside of the medical care system; forexample, community services such as home care,food supply (‘meals on wheels’) and transport, andresidential or nursing home care. Depending onhow care is organized, it may be difficult to make aclear distinction between social and medical care,and some ‘social care’ costs may still relate in partto medical care services, for example home nursingor nursing and medical care provided to care homeresidents.Indirect costsusually refer to production losseslinked to the person with the illness (arising fromimpaired productivity while working, sick leave, earlyretirement, or death). This type of indirect cost isgenerally less relevant in the context of dementia,
Top-down versus bottom-upapproachesIn a ‘top-down’ analysis, the total costs for a specificresource (for example, health care costs or socialsector costs) are distributed appropriately to differentconditions. Such studies are often based on datafrom local or national registers of service users. Withthe ‘bottom-up’ method, detailed cost data froma defined sub-population (often from a local area)are extrapolated to the ‘total’ dementia populationin a given country or region. One limitation of thisapproach is that not all costs linked to peoplewith dementia may be directly attributable to thatcondition. Comorbidity with other chronic diseases(such as stroke, heart disease or arthritis) is relativelycommon. However, recently published analysesfrom the 10/66 Dementia Research Group studies
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
13
where most of those affected are older peoplewho would in most cases be retired. The costs ofinformal care, arising from the unpaid inputs offamily caregivers, friends and others (see below) aremore often considered as indirect costs, but this is acomplicated issue(8,9).
costs, the corresponding figures are 11 out of 31studies.
The ideal scenario for computing costof illness … and the realityAn ideal worldwide CoI study has a societalviewpoint including comprehensive accountingof informal care, direct medical and social carecosts. Precise data on the prevalence of dementiaand resource utilization should be derived fromrepresentative population-based studies. Thesedata and the unit costs applied to the resourcesused should refer to the same index year. The samemethods should be used to collect these data acrossall countries.The reality is different:• Estimates of the size of the older population are ofvariable quality for different countries.• Data on dementia prevalence (the proportion ofthe older population affected) applied to the totalpopulation size to estimate the numbers of peoplewith dementia is not available for all countries(5).• Most studies of care arrangements andresource utilization for people with dementiause convenience rather than representativepopulation-based samples. Many of the estimatescome from small studies and, hence, may beimprecise. Many studies are not recent, andcare arrangements and patterns of healthcareutilization may change over time. For manycountries, there are few or no studies available,but informal care arrangements are likely to behighly dependent on culture and place.• Many basic indicators, for example demographicand macroeconomic data, are not yet providedfor 2010. However, projections can be found inonline databases.For all of the above reasons, it is necessary to relyon some degree of imputation (making an educatedand informed estimate when precise data are notavailable) and a range of assumptions. The CoIfigures that are presented here must be regarded asestimates rather that exact calculations.
The viewpointAny analysis of health economics has a viewpoint,even if this is not always made explicit. With asocietal viewpoint, which is recommended in mostcases, all relevant costs and outcomes should beincluded(10). However, the focus can be upon thecontributions of different payers; for example, localor national government, an insurance company,caregivers or patients (the latter referred to as ‘out ofpocket costs’). Above all, it is essential that there istransparency regarding the viewpoint adopted.
The representativeness of data sourceson resource utilizationStudies on resource utilization and costs associatedwith dementia typically use one of two mainapproaches for sampling: representative samplesfrom population-based studies or ‘convenience’samples of those receiving help from dementia careservices or Alzheimer associations. Studies aresometimes labelled as ‘population-based’ even ifthe recruitment process for the study is more or lessbased on clinical service contact. Naturally, peopleidentified through convenience sampling tend tohave more advanced and severe dementia, theircaregivers typically report higher levels of strain, andthe families are more likely to have accessed andto have used more health and community supportservices. If the aim is to characterise people affectedby the disease to the extent that they need and havesought formal care (‘users’ of care), then clinical-based study populations are sufficient. However,if the aim is to describe all people with the illness,then population-based studies including both thosewho use formal care and those that do not areneeded, otherwise average and total costs may beoverestimated. Since many reports, particularly thosewith a top-down design, include many sources, it isnot easy to judge whether the underlying sourcesin this Report are population based or clinical/userbased. Of the 42 studies that are used in this Reportfor estimating the costs of informal care, we regard11 studies as having population based designs(cohort studies, case control studies) or includingcontrols (people without dementia). For the direct
Alzheimer’S diSeASe iNTerNATioNAl
14
World Alzheimer reporT 2010
Methods used in our cost of illness analysesSummaryOur base case approach is a societal, prevalence-based gross CoI study in which country-specificannual per capita costs (direct medical and socialcare costs, and informal care) have been applied toestimated numbers of people with dementia in eachcountry (derived from the World Alzheimer Report2009(5)), and aggregated up to the level of WHOregions (see box), and World Bank country income-level groupings.• Most of the source papers (see below) providingevidence on direct medical and social care, andinformal care, have a bottom-up design. Mostused convenience sampling, although somedata were derived from more representativepopulation-based surveys.• The costs in the current Report (as well as theprevalence of dementia) reflect estimates for2010 and are expressed as US dollars. Costsestimates based on previous years are inflatedto 2010 using relevant country-specific data fromthe International Monetary Fund (IMF) or WorldEconomic Outlook (WEO)i, or if lacking fromthose sources, from the World Bankiior WorldFact Bookiii. Data on per capita Gross DomesticProduct (GDP) was obtained in a similar way.• To permit aggregation across countries, andcomparisons between countries and regions,costs are expressed as US dollars converted fromlocal currencies based on current exchange rates.An alternative approach based on purchasingpower parity (PPP) was used in the sensitivityanalysis (see page 28 for further details).To facilitate comparisons with previous studies, wealso present data according to current World Bankclassifications. Based on its Gross National Income(GNI) per capita, every economy is classified as lowincome, middle income (subdivided into lower middleand upper middle), or high income. Economies aredivided according to 2009 GNI per capita calculatedi World Economic Outlook Database [database on the Internet].IMF. 2010 [cited 2010-02-07]. Available from: http://www.imf.org/external/pubs/ft/weo/2010/01/weodata/weoselgr.aspxii Data Research [database on the Internet]. World Bank. 2010 [cited2010-06-07]. Available from: http://econ.worldbank.org/WBSITE/EXTERNAL/EXTDEC/0,,menuPK:476823~pagePK:64165236~piPK:64165141~theSitePK:469372,00.htmliii World Fact Book [database on the Internet]. 2010 [cited 2010-05-30]. Available from: https://www.cia.gov/library/publications/the-world-factbook/
CLassifiCatiOn Of COuntRiesin this Report, countries are classified accordingto the system that will be used in future GlobalBurden of disease reports from the World healthOrganization (WhO). a similar approach wasused in the World alzheimer Report 2009. theclassification is principally geographic, withseven sub-regions in asia (australasia, asiaPacific high income, asia Central, asia east, asiasouth, asia southeast and Oceania), three ineurope (europe Western, europe Central, europeeastern), six in the americas (north america,Caribbean, Latin america andean, Latin americaCentral, Latin america southern, Latin americatropical), and five in africa (north africa / middleeast, sub-saharan africa Central, sub-saharanafrica east, sub-saharan africa southern andsub-saharan africa West).
using the World Bank Atlas methodiv. The groupsare: low income, $995 or less; lower middle income,$996 – $3,945; upper middle income, $3,946 –$12,195; and high income, $12,196 or more.
The evidence on the prevalence ofdementia, and numbers affectedworldwideFor the World Alzheimer Report 2009(5), weconducted a systematic review of the globalprevalence of dementia, identifying 147 studies in21 Global Burden of Disease (GBD) world regions.Previous estimates of numbers of people withdementia worldwide, published inThe Lancetin2005(11), were based on expert consensus. A largenumber of new studies unearthed in the systematicreview, particularly from low and middle incomecountries, enabled us to conduct quantitative meta-analyses in 11 of the 21 GBD world regions. The newestimates showed that age standardised prevalence(for those aged 60 years and over) did not vary muchbetween world regions, with between 5% and 7%affected in most regions. The exceptions were thefour sub-Saharan African regions where between2% and 4% were affected. When compared with ourearlier ADI/Lancet consensus estimates, those foriv http://data.worldbank.org/about/country-classifications/world-bank-atlas-method
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
15
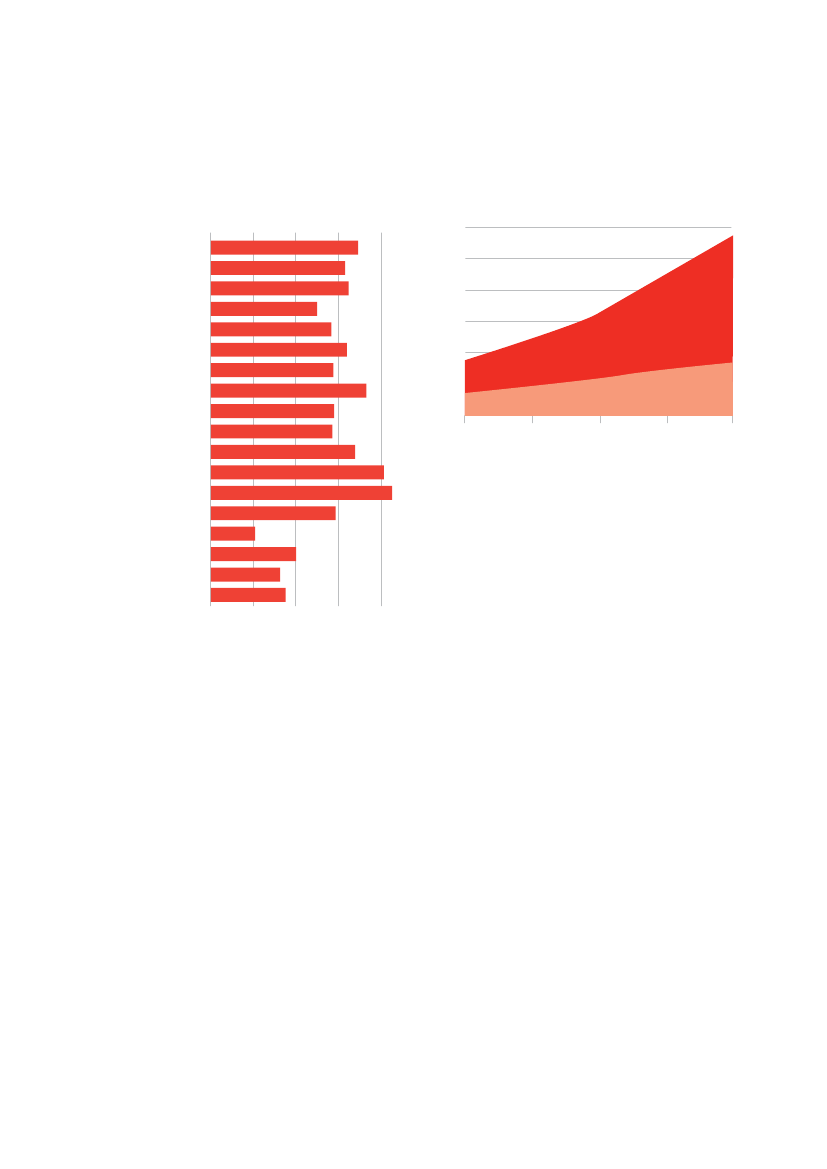
three regions were higher – western Europe (7.3% vs.5.9%), south Asia (5.7% vs. 3.4%) and Latin America(8.5% vs. 7.3%). Those for east Asia were lower(5.0% vs. 6.5%).Having applied these prevalence proportions tothe United Nations estimates of the total olderpopulation, we estimate 35.6 million people withdementia in 2010, with the numbers nearly doublingevery 20 years, to 65.7 million in 2030 and 115.4million in 2050. These figures represented a 10%increase on the figures published inThe Lancetin2005. 58% of all people with dementia worldwide livein low and middle income countries, rising to 71% by2050. Proportionate increases over the next twentyyears in the number of people with dementia willbe much steeper in low and middle compared with
high income countries. We forecast a 40% increasein numbers in Europe, 63% in North America, 77%in the southern Latin American cone and 89% inthe developed Asia Pacific countries. These figuresare to be compared with 117% growth in east Asia,107% in south Asia, 134-146% in the rest of LatinAmerica, and 125% in north Africa and the middleEast. Given that the new figures published in lastyear’s World Alzheimer Report are based on themost up to date and comprehensive review of theevidence base, we believe these to be the mostrobust and valid figures currently available.
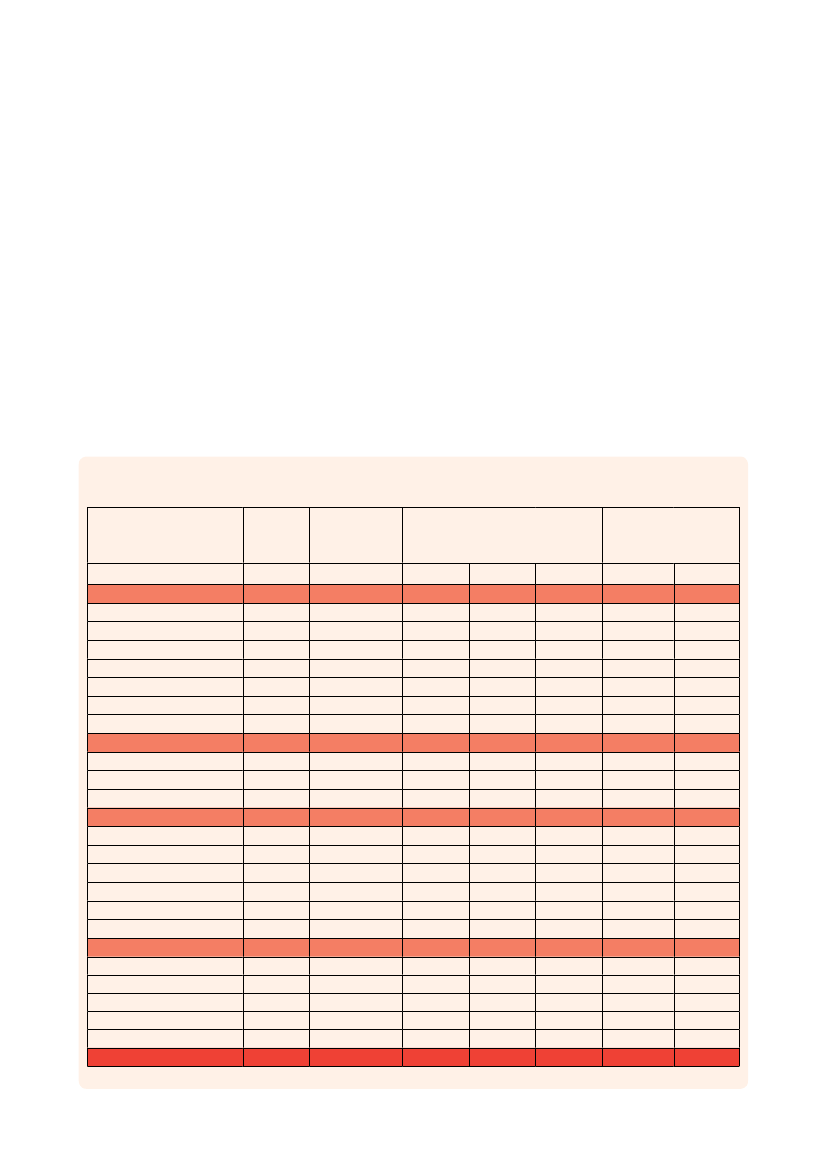
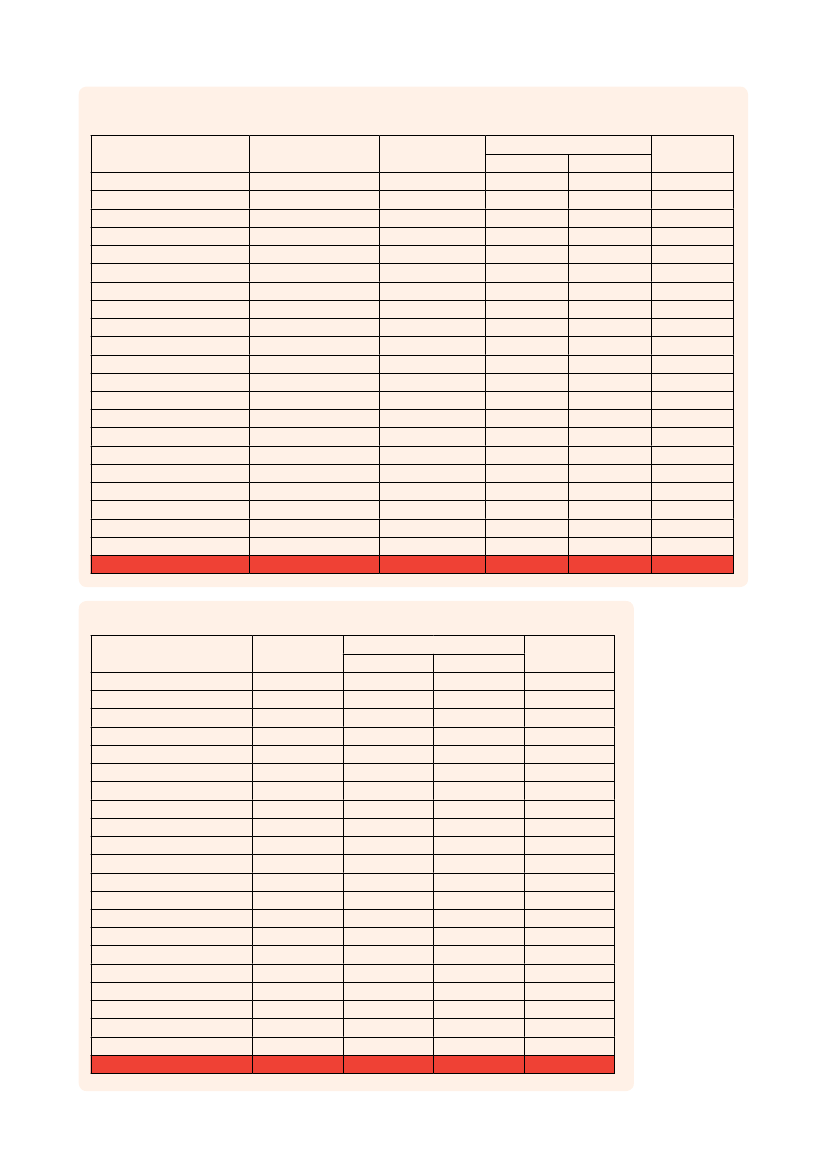
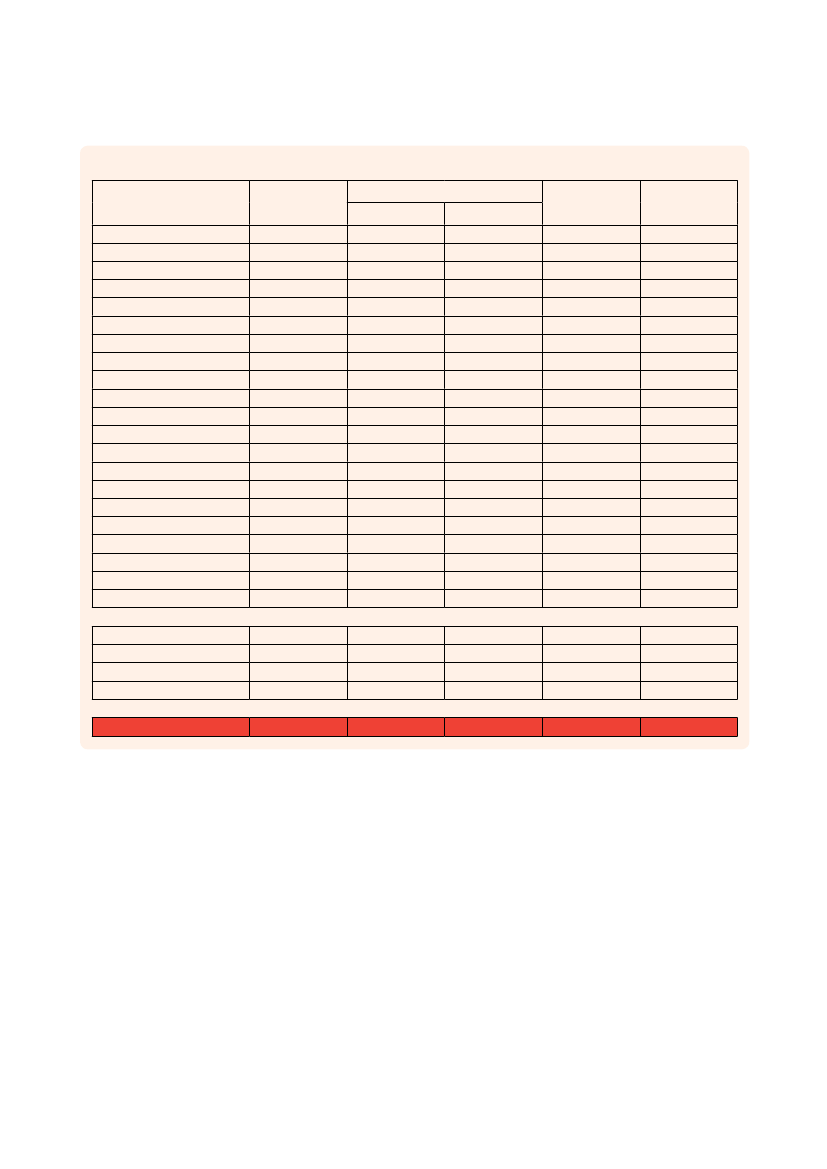
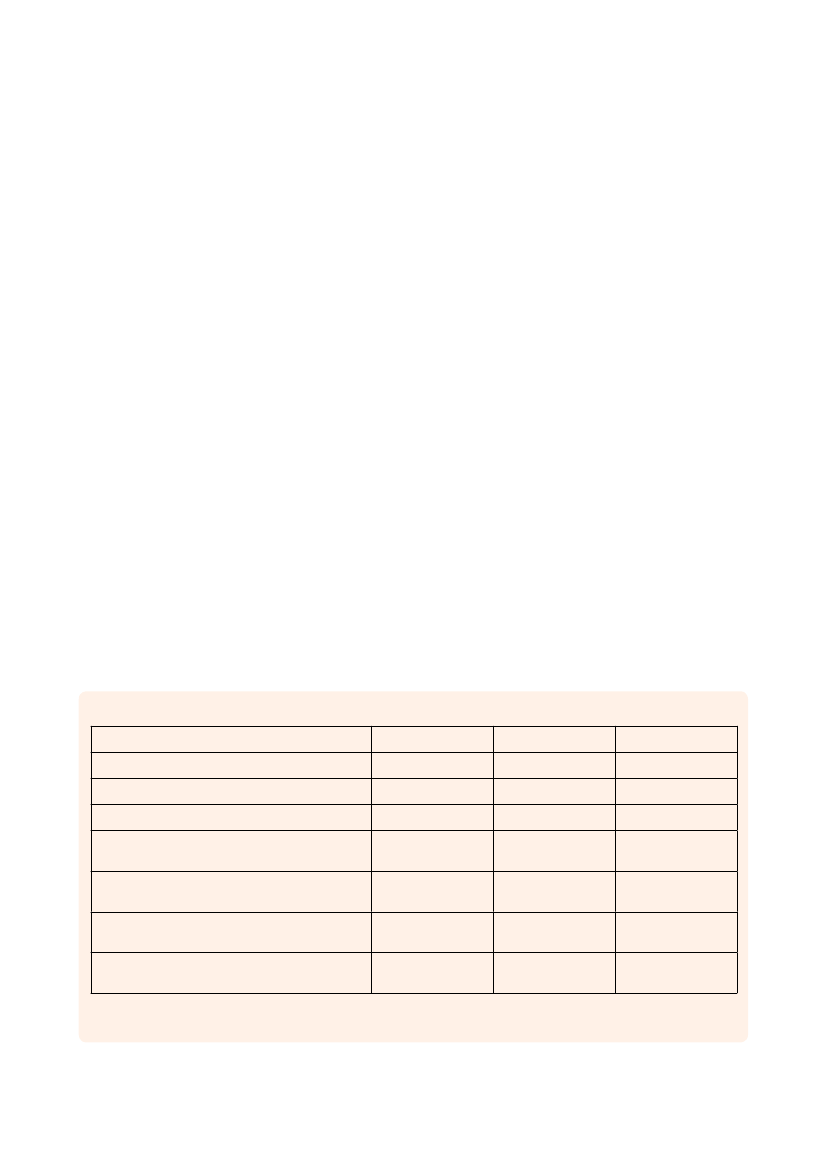
Table 1Total population over 60, crude estimated prevalence of dementia (2010), estimated number of people withdementia (2010, 2030 and 2050) and proportionate increases (2010-2030 and 2010-2050) by GBD world regionOver 60Crudepopulationestimated(millions) prevalence (%)2010ASIAAustralasiaAsia PacificOceaniaAsia, CentralAsia, EastAsia, SouthAsia, SoutheastEUROPEEurope, WesternEurope, CentralEurope, EastTHE AMERICASNorth AmericaCaribbeanLatin America, AndeanLatin America, CentralLatin America, SouthernLatin America, TropicalAFRICANorth Africa / Middle EastSub-Saharan Africa, CentralSub-Saharan Africa, EastSub-Saharan Africa, SouthernSub-Saharan Africa, WestWORLD406.554.8246.630.497.16171.61124.6151.22160.1897.2723.6139.30120.7463.675.064.5119.548.7419.2371.0731.113.9316.034.6615.33758.5420103.96.46.14.04.63.23.64.86.27.24.74.86.56.96.55.66.17.05.52.63.71.82.32.11.24.7Number of people with dementia(millions)201015.940.312.830.020.335.494.482.489.956.981.101.877.824.380.330.251.190.611.051.861.150.070.360.100.1835.56203033.040.535.360.040.5611.939.315.3013.9510.031.572.3614.787.130.620.592.791.082.583.922.590.120.690.170.3565.69205060.920.797.030.101.1922.5418.1211.1318.6513.442.103.1027.0811.011.041.296.371.835.548.746.190.241.380.200.72115.38Proportionateincreases (%)2010-2030 2010-20501077189100701171081144044432689638813613477146111125719270948528215714840026131130434987939166246151215416435200428370438243283100300225
GBD Region
Alzheimer’S diSeASe iNTerNATioNAl
16
World Alzheimer reporT 2010
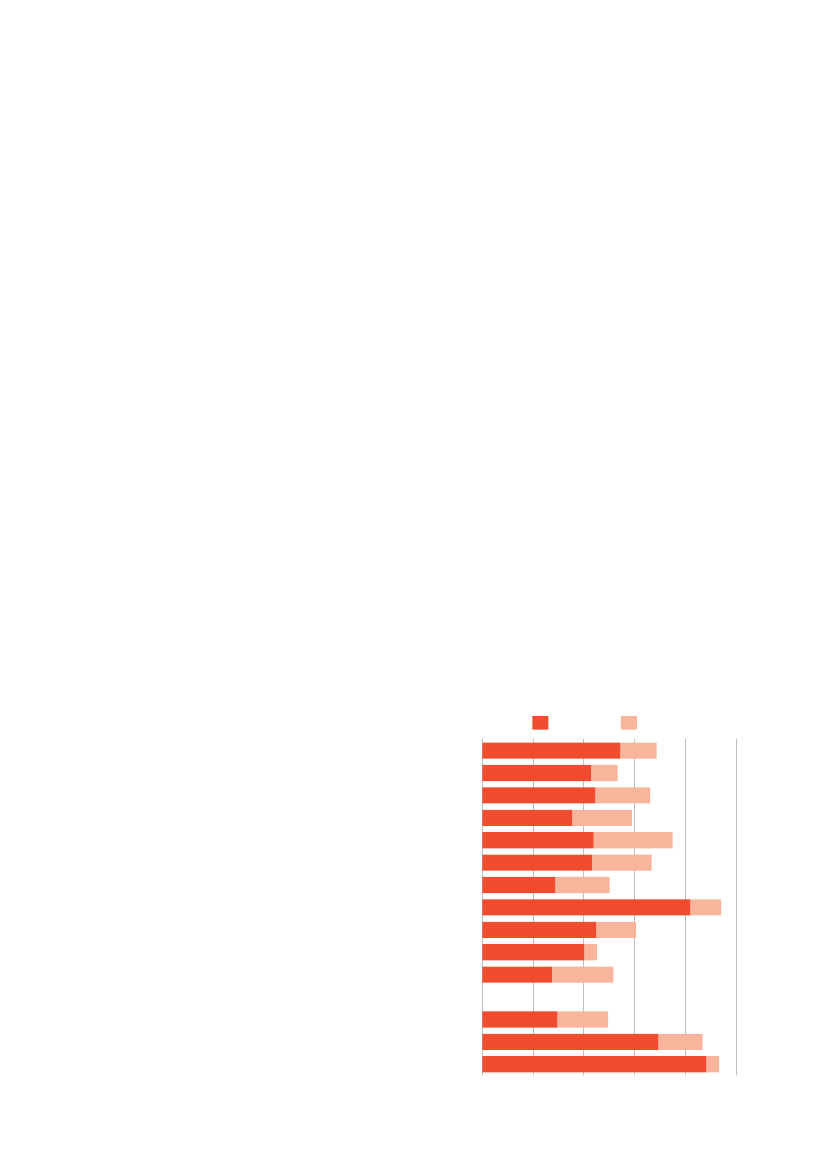
Figure 2Estimated prevalence of dementia for those aged60 and over, standardised to Western Europe population, byGBD region (%)Standardised prevalence %0AustralasiaAsia PacificOceaniaAsia EAsia SAsia SEAsia CentEurope WEurope CentEurope EAmerica NCaribbeanLatin AmericaN Africa/ Middle EastSub-Saharan Africa WSub-Saharan Africa ESub-Saharan Africa CentSub-Saharan Africa S2468
Figure 3The growth in numbers of people with dementia inhigh income countries and low and middle income countriesNumbers of people with dementia (millions)120100806040200201020202030Year20402050low and middleincome countries
high income countries
The evidence on the utilization ofmedical and social care, and informalcareseaRCh stRateGyFor the previous Cost of Illness (CoI) estimates for2005 and 2009(12,13), a comprehensive literaturesearch was done. The resulting database has beenupdated and refined for the present Report. Forthe cost data, we focused on papers and reportsno older than 2000, although older studies wereconsidered for countries where there was no newerdata. Older studies were also accepted regardingthe amount of informal care. The key criterion wasthat direct and indirect costs as well as amountsof informal care could be identified. The searchwas done in PubMed/Medline, Ingenta, CochraneLibrary, NHSEED/HTA, HEED, EMBASE, Currentcontents, PsycINFO, ERIC, Societal servicesabstracts and Sociological abstracts. The searchterms (MESH/Subheadings when appropriate) weredementia/Alzheimer’s disease/Alzheimer diseasecombined with cost and/or economic and informalcare. Two recent systematic reviews comprising
published papers between 1969 and 2008 with atleast an abstract in English were also included(14,15).Secondary papers from reference lists wereconsidered for inclusion. Another source was variousreports that were not found in scientific databases,such as reports from governmental authorities andAlzheimer associations.imPutatiOn aPPROaChesOur general aim was to generate evidence-basedestimates of resource utilization for each country.Where more than one estimate was available for agiven country we selected the one that we regardedto be the most appropriate study. Where no estimatewas available we first used estimates from othersimilar countries within the same region, or, failingthat, adjacent regions. For particular resources, forcertain regions, more complex procedures wereused and these are described in the relevant section.diReCt COstsData on direct costs were available from 21 countriesrepresenting 49% of the worldwide dementiapopulation (Argentina, Australia, Belgium, Canada,
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
17
China, Denmark, Finland, France, Germany, Hungary,Ireland, Israel, Italy, Korea, New Zealand, Norway,Spain, Sweden, Turkey, UK and USA). For manycountries, there were no available data on directcosts. For each country, we sought to estimateboth total direct costs and the distribution betweendirect medical and social care costs. Regionalimputation from local similar countries was possiblefor a further 74 countries representing 27% of theworldwide dementia population, mainly in Europebut also in Latin America. For the remaining 24%of the dementia population, in 97 countries mainlyin Africa and Asia, no data was available even fromneighbouring countries. From macro-economicresearch it is known that there is a strong correlationat country-level between per capita expenditure onhealth care and per capita Gross Domestic Product(GDP). This relationship can be used to impute directcare costs by assuming that these costs per personwith dementia as a proportion of GDP per capitafor the countries and regions where imputationis necessary are similar to the proportions in thecountries for which cost data are available(12). Ina simple linear regression model, the relationshipbetween the costs per person with dementia andyear and the GDP per person and year was tested.Based on this model (derived from 31 papers(16-46)),for each US$1 increase in annual per capita GDP theannual cost per person with dementia increased byUS$0.37 (p<0.001, r2=0.43, 95% confidence interval0.22-0.51). The regression approach did not workwell for the estimation of the distribution betweendirect medical and direct non medical costs, and sothe percentage distribution observed in one country(China) was used to specify the likely distribution forall countries within the Asian and African regions forwhich these data were not directly available.infORmaL CaReFamily members, friends and others who take oncaring roles are likely to experience role strain,negative impacts on their physical and mentalhealth, and their quality of life, and consequentchanges to their social network(47-51). Their inputshave an important influence on the societal costs ofdementia, since they are producers of an extensiveamount of unpaid informal care(52-57). However,translating this contribution into economic costs isnot straightforward.
• Assistance with basic activities of daily living(ADL), such as eating, dressing, bathing, toileting,grooming, and getting around – sometimesreferred to as personal care.• Assistance with instrumental activities of dailyliving (IADL), such as shopping, preparing food,using transport, and managing personal finances.• Supervision to manage behavioural symptoms orto prevent dangerous events(53).Personal care is relatively easy to assess andinterpret across countries and cultures, but thenature and relative importance of IADLs are likelyto be much more culture-specific. Furthermore, theperson with dementia and the caregiver may eachcontribute to the performance of these activities, forexample shopping (referred to as ‘joint production’).Second, costing informal care is also complicatedand controversial(8,58-64). Two methods are frequentlyused, the ‘opportunity cost’ and the ‘replacementcost’ approaches. Informal care is unpaid. Insome high income countries there are systems tocompensate or remunerate family caregivers, but theamounts concerned are relatively small. However,whether a caregiver is paid or unpaid does not affectthe economic valuation of their inputs. Payments andother transfers have an impact on the distribution ofthe economic burden but not on the total societalcost. To calculate the opportunity cost it is firstnecessary to identify the possible alternative use ofthe caregiver’s time. If the alternative is working onthe labour market – as may be the case, especiallyfor younger caregivers who often give up or cut backon work to provide care – then the cost for informalcare should be valued according to the productionloss due to absence from work. More challengingis the costing of caregiver time for retired people(as is often the case with spouses of people withdementia). There is no obvious answer to how thisshould be calculated, since there are no obviousmarket prices(62). ‘Willingness to pay’ approachesmay be an option(65, 66). The replacement costapproach assumes that the informal caregiver’sinputs should be calculated according to the cost ofreplacing them with a professional caregiver.Third, some people with dementia live in carehomes, where professional staff provide mostcare, and informal care is less relevant. These maybe residential care homes (providing low intensitycare, with few trained staff), or nursing homes(providing high intensity care with more trained
First, quantifying caregiver time is problematic. Theinputs most commonly assessed are:
Alzheimer’S diSeASe iNTerNATioNAl
18
World Alzheimer reporT 2010
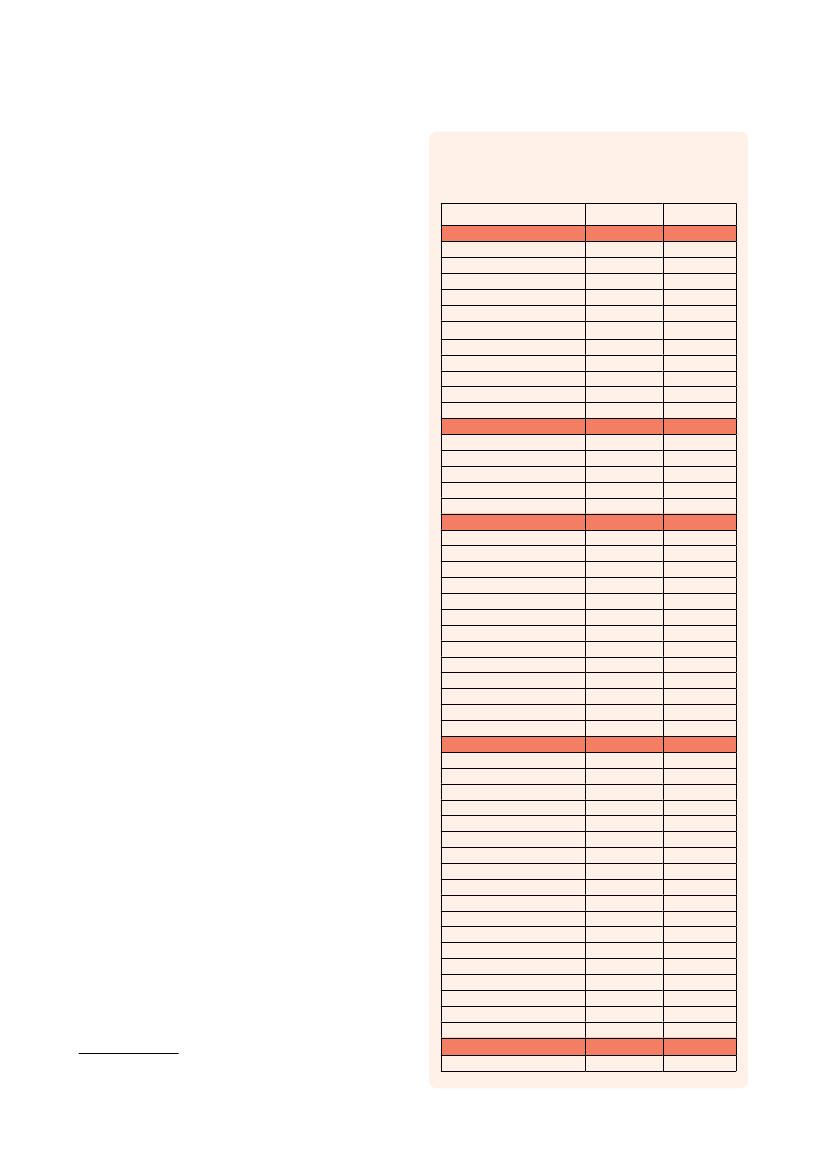
nursing and medical staff), or specialist facilitiesfor dementia care. There are few reliable estimatesof the proportion of people with dementia living inthese facilities, as opposed to their own homes inthe community. Estimates for the United Kingdomvary between 35 and 50%(36,67,68), while for Canadathe estimate was 45-50%(16,69). In settings in highincome countries, people with dementia residingin care homes contribute a substantially higheramount to the total cost of illness than in low andmiddle income countries. In low and middle incomecountries, anecdotal information suggests thatfew such facilities exist, and that the large majorityof people with dementia are cared for, informally,in the community. In order to estimate total costsaccurately and to apportion costs appropriatelywithin sectors, it is crucial to estimate the relativeproportions of people with dementia living at homeor in a long-term residential or nursing home carefacility. In most countries, there is no publisheddata on this. So, for the purpose of this Report, ADIcommissioned a worldwide questionnaire surveyof key informants (including Alzheimer associationstaff, ADI’s Medical and Scientific Advisory Panelmembers and 10/66 Dementia Research Groupprincipal investigators) to provide more informationon this issue. Informants were asked, in their opinion,what proportion of people with dementia residedin care homes, in both city areas and rural areas.The questions had fixed 10% point range responseintervals (and one 100% option). The range ofestimates is wide from some countries, since severalrespondents had answered. Extreme outliers (8respondents out of 86) were excluded. Two trendsare obvious: the proportion of people with dementiaresiding at home is higher in low income countriesand higher in rural areas (table 2). In high incomecountries, the mean proportion living at home is66% (95% confidence interval 64%-68%), while inlow and middle income countries 94% of peoplewith dementia live at home (95% confidence interval92%-96%).For the estimates in the cost model, we used thecentral values (after excluding outliers). Imputationwas used for nearby countries with similar carestructures. From a UN demographic database wegathered information on the rural-urban populationdistributions for all relevant countriesi, whichcombined with the results from the ADI questionnairei World Urbanization Prospects The 2009 Revision [database onthe Internet]. UN. 2009 [cited 2010-05-25]. Available from: http://esa.un.org/unpd/wup/index.htm
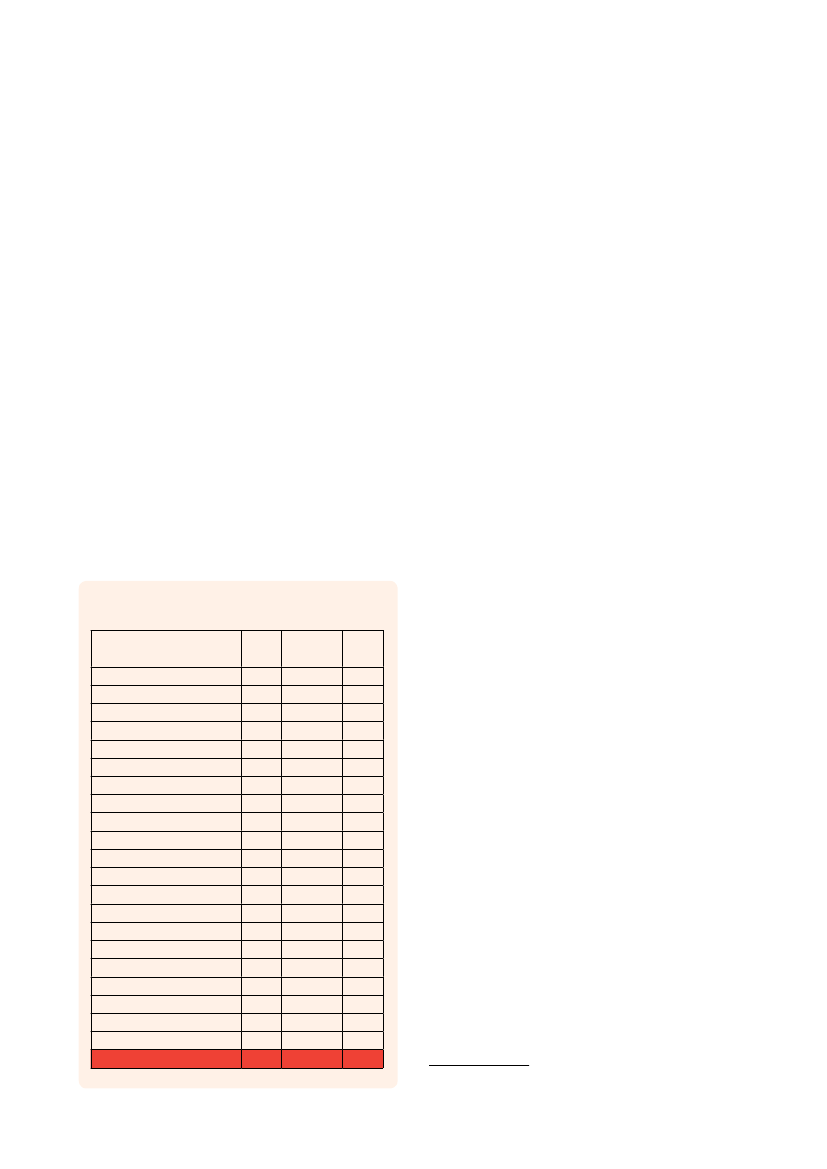
Table 2Estimated proportion of people with dementiathat are living at home (%).Source: ADI survey (unpublished)CountryASIAArmeniaChinaIndiaJapanJordanPakistanNepalSingaporeSri LankaThailandTurkeyAFRICAEgyptMauritiusNigeriaSouth AfricaZimbabweAMERICASArgentinaArubaBahamasBoliviaBrazilDominican RepublicHondurasJamaicaMexicoPeruPuerto RicoVenezuelaUnited StatesEUROPEBelgiumCroatiaCyprusGermanyGreeceIrelandIsraelItalyMacedoniaFormer Yugoslav Rep. ofNetherlandsPolandRomaniaSerbiaSlovakia (Slovak Republic)SloveniaSwedenSwitzerlandUnited KingdomAUSTRALASIAAustraliaUrban areas Rural areas50-59%70-99%90-94%60-79%95-99%100%100%90-99%70-99%80-89%70-79%100%80-89%80-89%90-94%70-79%50-89%80-89%95-99%70-94%70-94%90-94%95-99%70-79%80-99%90-94%70-79%90-94%70-79%50-59%80-89%70-79%50-59%80-89%60-69%80-89%50-59%50-59%60-69%80-89%80-89%95-99%80-89%40-49%50-59%60-69%50-94%50-69%50-59%80-94%95-99%70-79%95-99%100%100%100%95-100%95-99%90-94%100%80-89%90-94%100%95-99%70-94%80-89%95-99%90-99%90-99%95-99%100%70-79%95-100%95-99%70-89%95-99%80-89%70-79%95-99%95-99%60-69%95-99%60-69%80-89%50-59%90-94%70-79%95-99%100%100%90-94%60-69%50-59%50-59%50-94%50-69%
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
19
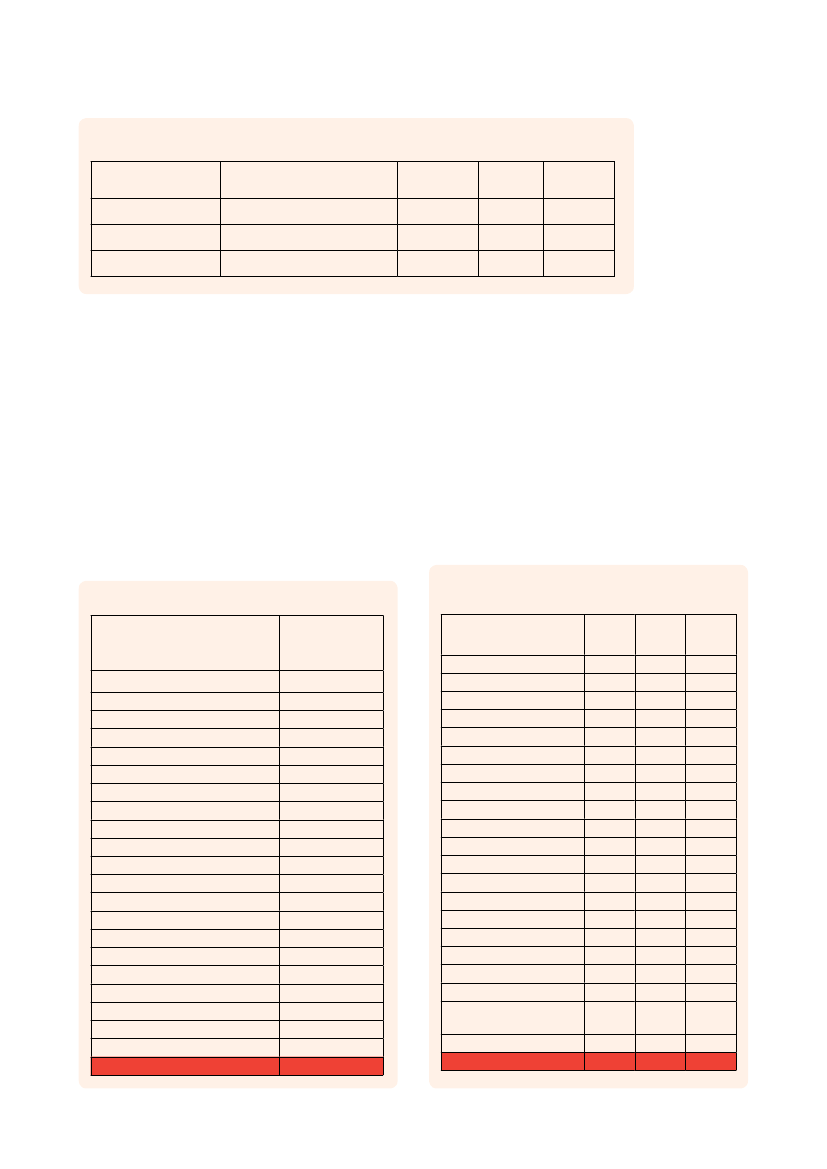
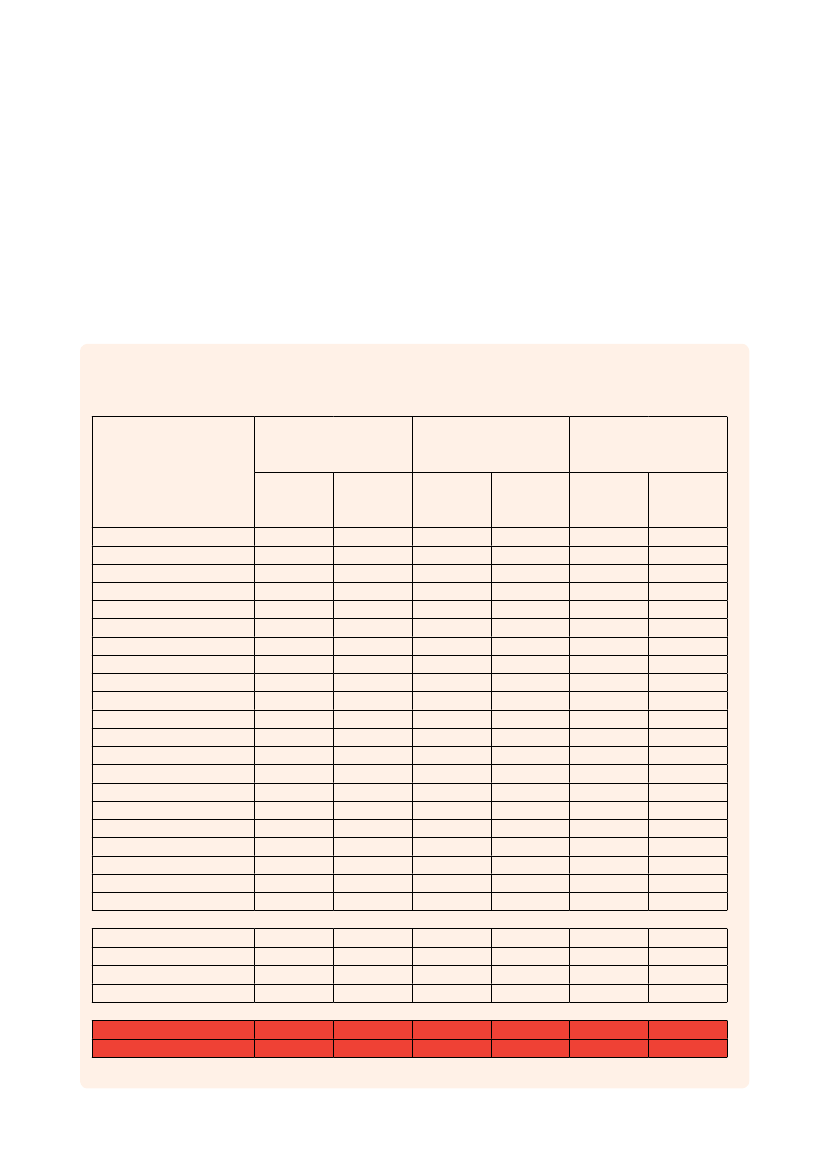
gave a weighted proportion of people with dementialiving at home in the community, and hence likely tobe in receipt of informal care.Based on our review of the international literature, weidentified:• 10 appropriate studies where time spent assistingwith basic ADLs was quantified, covering 25countries representing 63% of the worldwidedementia population(5,32,33,37,38,56,70-73).• 42 papers or reports with time spent assistingwith basic ADLs and IADLs combined, covering30 countries representing 73% of the worldwidedementia population(5,21,30-33,35-38,41,43,44,46,52,54-57,70-92).• 13 papers or reports with estimates of timespent in supervision, covering 25 countriesrepresenting 63% of the worldwide dementiapopulation(5,30,31,33,38,52,56,71-73,79,88,89).Regional imputation was carried out for theremaining countries according to the procedurespreviously described (page 16). However, for allTable 3WHO-region specific figures of informal careinputs (hours per day)WHO region(red=imputed)AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
African regions, global average figures were used.Although the degree of imputation required wasquite substantial, this still represents a considerableadvance on the evidence base available for previousreports, since to a large extent we were able touse region-specific figures. The detailed estimatesfrom six Latin American countries, India and China,where research is being done by the 10/66 group,provided important data from low and middle incomecountries for this review, which was not available forprevious worldwide cost estimates.The WHO-region specific estimates for informalcare inputs are summarised in table 3. Despite theproblems, noted above, in quantifying caregivingtime spent assisting with IADL, we used thecombined ADL figures (combining basic ADL andIADL care inputs) as the base option for calculatingthe costs of informal care. Our justification wasthat support for IADLs is an important part ofthe caregiver’s life with a person with dementia,and that there are many more papers describingcombined ADLs than those covering only basic ADLcare inputs. Cost estimates generated only fromassistance with basic ADLs (personal care), andfrom all categories of informal care (assistance withbasic ADLs, IADLs and supervision) are part of thesensitivity analysis.The base option for costing informal care for thisReport uses the opportunity cost approach, valuinginformal care by the average wage for each country .Since not all average wage figures were expressedas an hourly rate, a division factor of 8 was used fordaily wage figures, 40 for weekly and 172 for monthlywage figures. Average wage figures were availablefor 131 countries, covering 96% of people withdementia worldwide. This method may, arguably,overestimate costs arising from the contributions ofthose who would not normally form part of the labourforce, for example retired spouses. However, from aglobal viewpoint, it is necessary to use sources thatare globally available, in this case the InternationalLabour Organisation (ILO) / Laborsta database. Inthis database, income data is available for differentperiods (for example, International StandardIndustrial Classification of all Economic Activities(ISIC) rev 2, rev 3) and for different sectors (suchas agriculture, manufacturing) as well as a ‘Total’estimate representing all sectors economic activity.Not all of these data were available for all countries. Ifi
Basic Combined Super-ADLADLvision2.02.03.61.23.61.31.31.12.12.12.13.02.91.92.92.91.12.02.02.02.02.03.33.64.62.74.72.72.73.54.44.44.03.02.91.94.42.91.43.63.63.63.63.62.62.61.23.31.22.62.63.33.43.42.82.12.63.12.62.62.62.62.62.62.62.6
i Laborsta Internet [database on the Internet]. ILO. 2010 [cited2010-02-23]. Available from: http://laborsta.ilo.org/STP
Alzheimer’S diSeASe iNTerNATioNAl
20
World Alzheimer reporT 2010
Table 4
Comparisons between different average wage alternativesISIC categoriesISIC rev 2: 2-9ISIC rev 3: C-QManufacturing (ISIC rev 2 and 3)
1999-2008Total (ISIC rev 2 and 3)Total (ISIC rev 2 and 3)Total (ISIC rev 2 and 3)
Number ofcomparisons17250383
Meanratio1.081.031.00
95% CIfor ratio1.03-1.121.02-1.030.98-1.02
a ‘Total’ estimate was not provided, we used differentsummaries representing many, but not all sectors(including sectors 2-9 with ISIC rev 2 and sectorsC-Q for ISIC rev 3), and if those were lacking, weused data for the manufacturing sector (sector 3 withISIC rev 2 and sector D with ISIC rev 3). To assessthe possible effect of using different data sourcesto estimate average wage, we estimated the ratiobetween earnings per month calculated from ‘Total’(all sectors), most sectors (C-Q from ISIC rev 3 or2-9 from ISIC rev 2) or manufacturing only (both ISICrev 2 and 3), for countries where each of these data
sources was available (table 4). Our conclusion is thatadjustments are not necessary.For some countries, particularly in Africa, there wereno figures about hourly wage available at all. Forthese countries, imputation was done, based oncountries where hourly wage figures were availablefrom the same WHO region. The imputation wasadjusted according to the GDP per person fromcountries in the same WHO region with as similarGDP figures per person as possible. This imputationis examined in the sensitivity analysis.
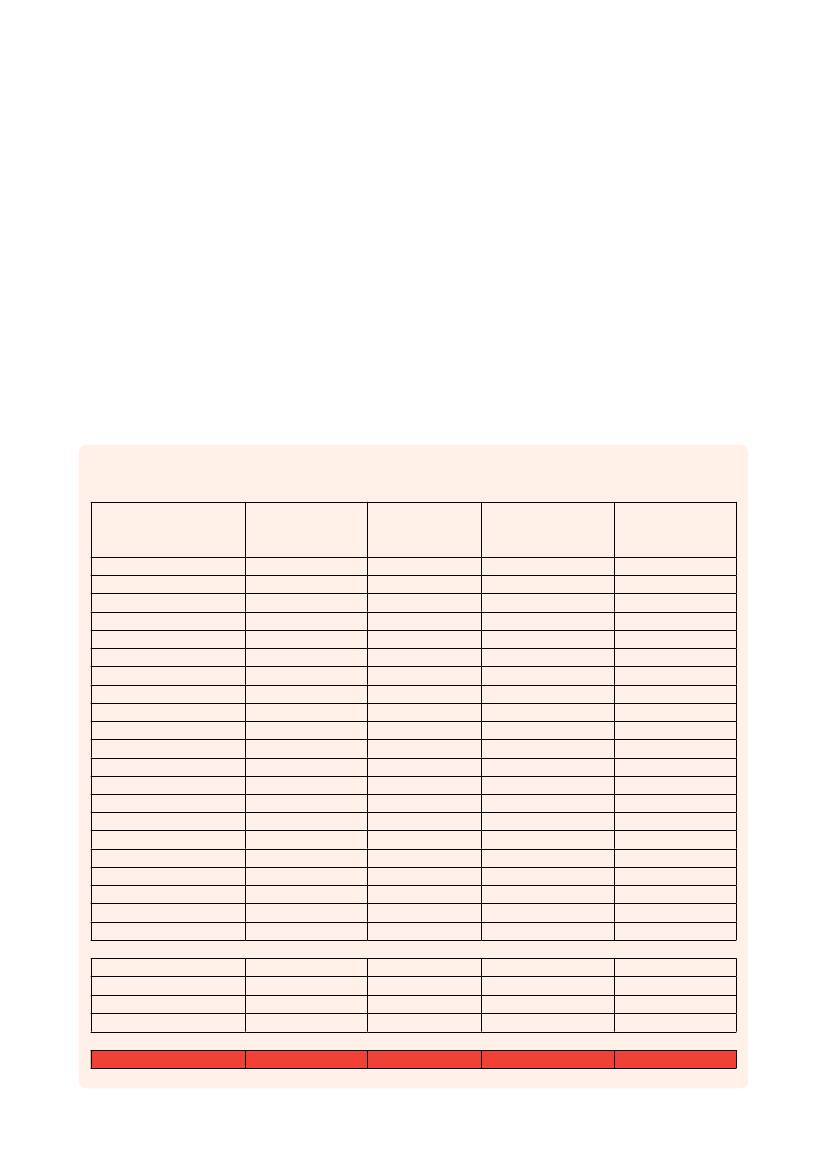
Table 5
Sex of caregivers, by WHO regionProportion (%)of caregiversthat are female72%81%55%71%55%77%86%66%74%82%71%80%85%82%74%91%71%81%81%81%81%67%
Table 6Sex differences in average wage in differentWHO regionsWHO region(red=imputed)AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan AfricaSouthernSub-Saharan Africa WestAll
WHO region(red=imputed)AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
Menvs All1.081.111.081.241.201.041.081.081.071.171.031.031.101.101.101.081.021.041.041.111.041.06
Women Womenvs All vs Men0.890.670.840.710.800.840.840.890.930.850.890.970.820.820.820.880.900.990.990.830.990.850.830.600.780.580.670.810.780.830.870.720.870.940.740.740.740.820.880.960.960.750.960.80
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
21
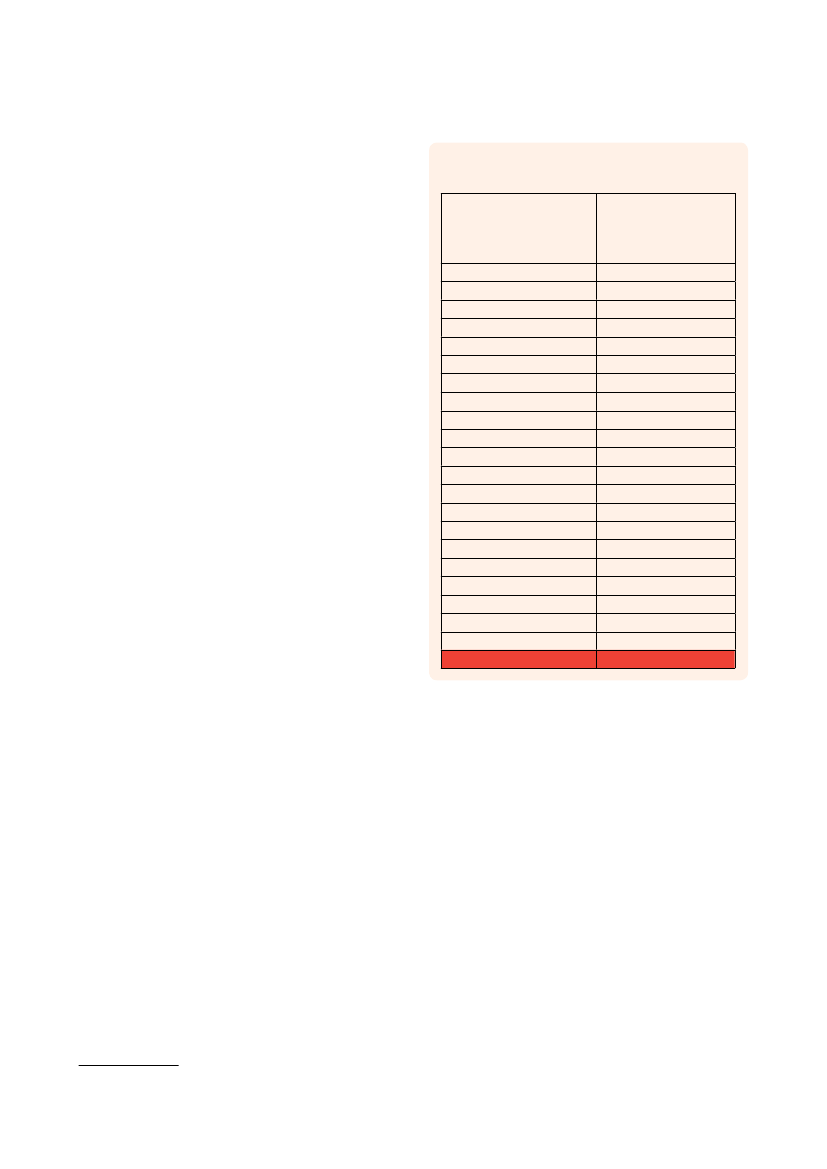
Since, in many countries, average wages forwomen are lower than those for men, we neededto determine the cost of care by male and femalecaregivers separately. In our review of the literatureregarding care arrangements for people withdementia (25 studies representing countries with78% of the global dementia population) we foundthat a woman was identified as the main informalcaregiver for 55-91% of people with dementia(table 5)(5,21,26,37,38,42,45,72,84,92-107).We looked at the ILO databaseito assess themagnitude of average wage differences betweenmen and women (table 6), which, when applied to theproportion of caregivers of each sex allowed us tocalculate an appropriately weighted hourly cost foreach WHO region. For some regions, imputation wasused with data from the nearby WHO region.We have also included an option in the sensitivityanalysis, varying the opportunity costs of caregiverinputs where care is provided by spouses, since theymight be assumed often to be retired or otherwisenot usually economically active. For these sensitivityanalyses, on an ad hoc basis, we valued these inputsat 25% and 50% of the average wage, applied toother non-spouse caregivers. From the caregiverliterature(5,21,26,30,31,37,38,42,45,49,55,57,72,84,89,92,93,96-102,108-112)spouses are the main caregivers for around40% of people with dementia, but with importantregional differences as seen in table 7.
Table 7Relation of informal caregiver to person withdementia by WHO regionProportion (%) ofmain caregivers thatare spouses of theperson with dementia43%36%41%38%40%24%8%48%36%36%52%18%15%8%46%54%38%41%41%41%41%41%
WHO region(red=imputed)AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
Sensitivity analysisSince CoI studies depend on a set of sources andassumptions, there are always uncertainties in CoIestimates. To consider the impact of the significantuncertain background factors, we have conducteda comprehensive set of sensitivity analyses in whichwe use different source data or vary assumptionsto see how this would have affected the results.However, another component of the sensitivityanalysis is to highlight the fact that there aredifferent views of what should be included in a CoIestimate and how to do it, for example regardinginformal care. There are several presentations in thesensitivity analysis to facilitate comparisons withother studies and approaches.
i Laborsta Internet [database on the Internet]. ILO. 2010 [cited2010-02-23]. Available from: http://laborsta.ilo.org/STP
Alzheimer’S diSeASe iNTerNATioNAl
22
World Alzheimer reporT 2010
References for Methods are combined withreferences for Results, page 34
Alzheimer’S diSeASe iNTerNATioNAl
23
World Alzheimer report 2010
Results
At the Alzheimer’s Cote d’Azur Christmas party, Amelia andher son pierre listened to the singers with interest. pierre is notmarried and lives next door to his mother, who he adores.
Alzheimer’S diSeASe iNTerNATioNAl
24
World Alzheimer reporT 2010
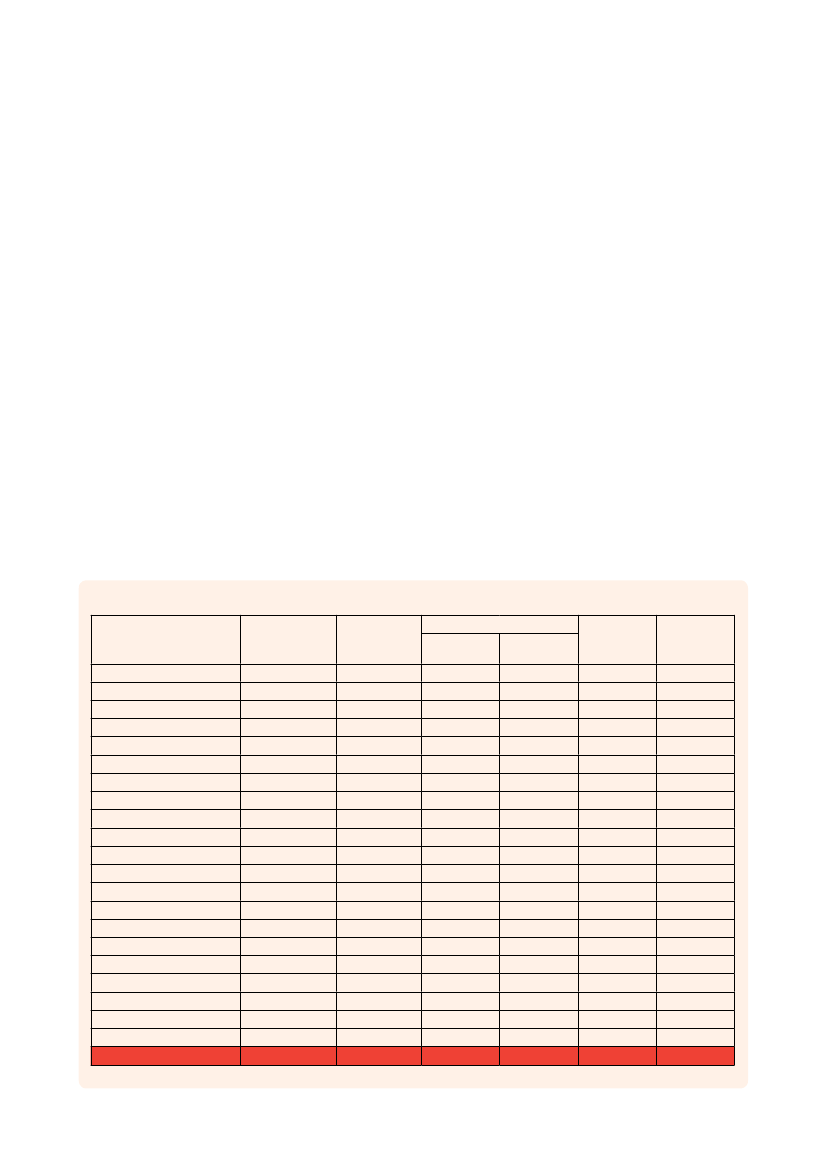
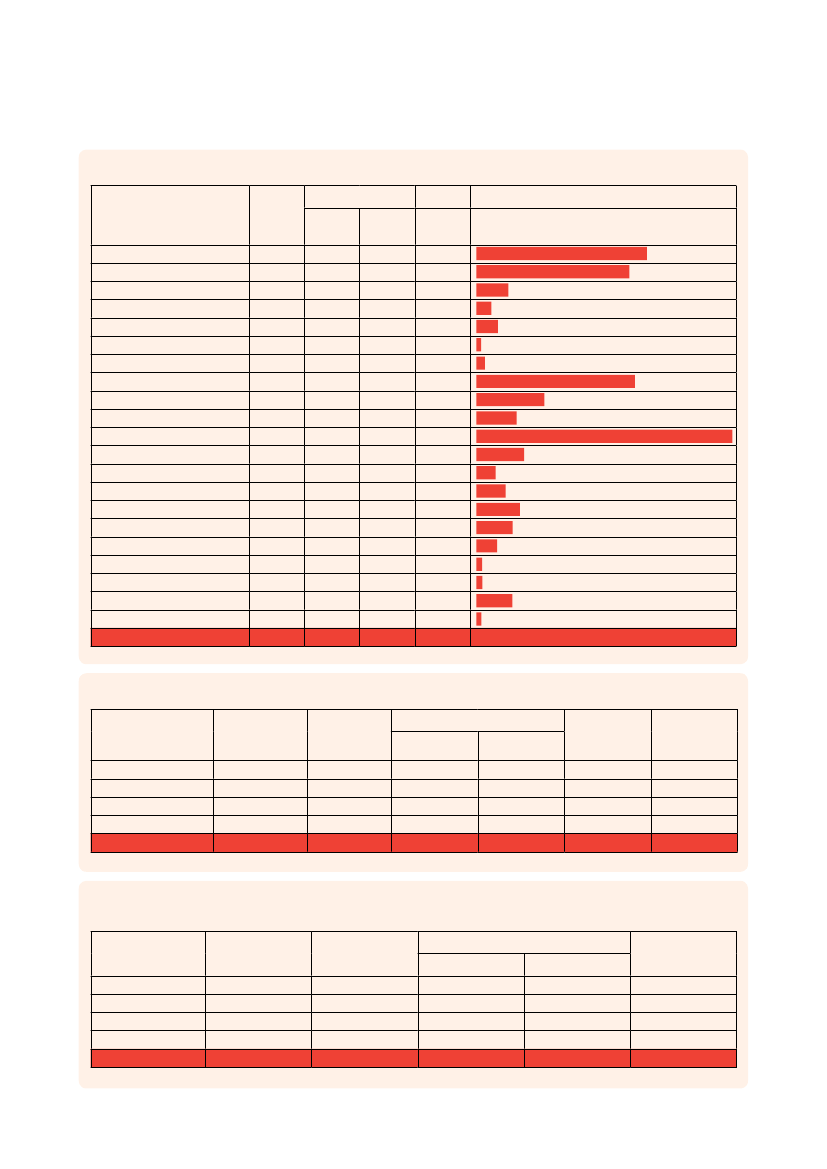
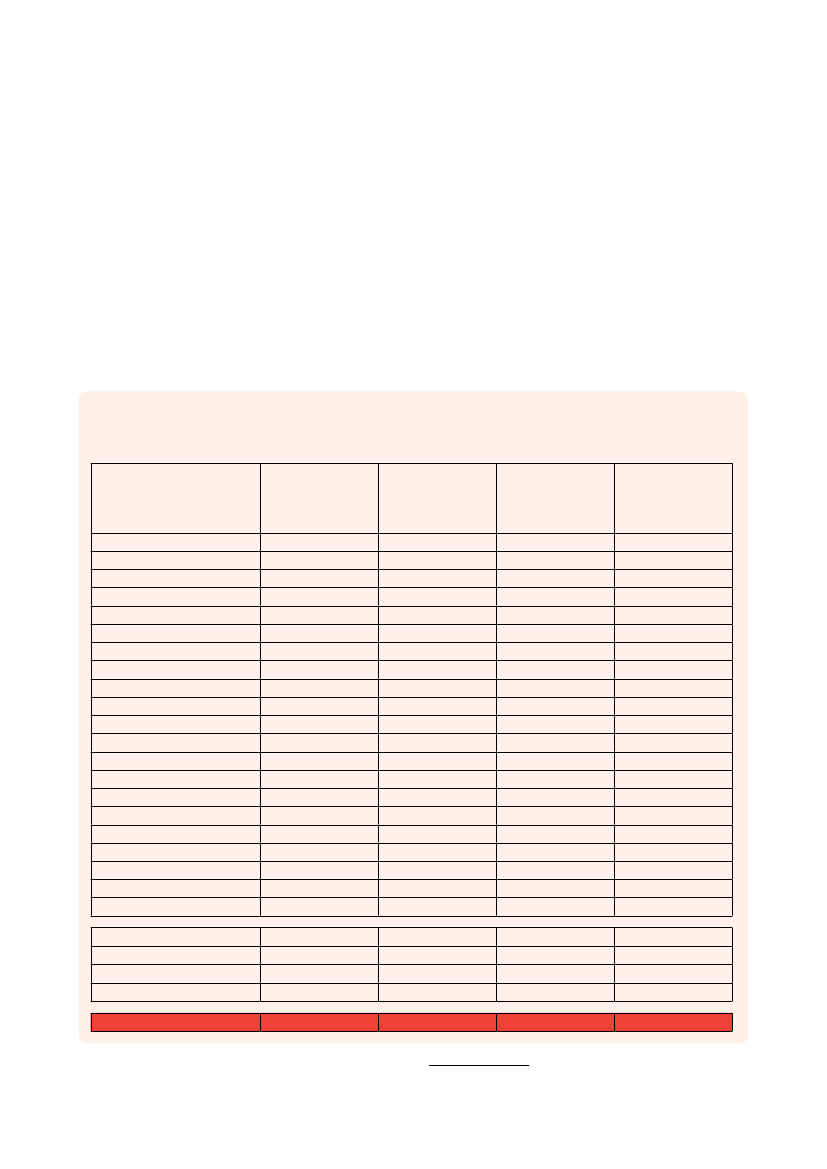
resultsResults of base optionThe total estimated worldwide costs of dementiaare US$604 billion in 2010 (table 8). About 70%of the costs occur in Western Europe and NorthAmerica (table 9). Costs of informal care and thedirect costs of social care generally contribute similarproportions of total costs, while the direct medicalcosts are much lower (table 10). However, in low andmiddle income countries direct social care costs arenegligible and informal care costs predominate. Theresults of the base option are seen in tables 8–15.The cost per person with dementia is highest inNorth America (US$48,605 – table 11) and lowestin the South Asia region (US$903 – comprisingcountries such as India and Bangladesh) andWestern Sub Saharan Africa (US$969). The costper person with dementia is therefore more than 50times higher in the richest world regions than in thepoorest.The differences between developed and developingcountries are even more obvious when the WorldBank classification is applied (tables 12-15). Lowincome countries, where 14% of people withdementia reside, contribute less than 1% of the totalcosts (table 13).The costs of informal care constitute the majority ofcosts in the low income and lower middle-incomecountries while the direct costs of social care have amuch larger role in the high income countries (table14), probably due to the costs of long term residentialand nursing home care in these countries.The total cost per person with dementia is 38 timeshigher in high income countries than in low incomecountries, and the direct costs of social care are 120times higher (table 15).
Table 8
Aggregated costs in each WHO region (billions US$)Number ofpeople withdementia311,3272,826,38816,553330,1255,494,3874,475,3242,482,0766,975,5401,100,7591,869,2424,383,057327,825254,9251,185,559614,5231,054,5601,145,63367,775360,602100,733181,80335,558,717Informal care(all ADLs)4.3034.600.070.4315.242.311.7787.058.597.9678.761.500.351.582.362.171.900.040.280.520.11251.89
Direct costsMedical0.705.230.020.284.331.161.4830.192.673.4236.830.780.312.611.422.672.050.020.080.110.0496.41
Social5.0742.290.010.242.840.570.7392.882.942.9497.450.710.282.371.292.420.540.010.040.060.02255.69
Total costs10.0882.130.100.9422.414.043.97210.1214.1914.33213.042.980.936.565.077.264.500.070.400.690.18603.99
Percentof GDP0.97%1.31%0.46%0.36%0.40%0.25%0.28%1.29%1.10%0.90%1.30%1.06%0.43%0.37%1.02%0.42%0.16%0.06%0.17%0.24%0.06%1.01%
AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestTotal
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
25
Table 9The contribution of each WHO region to the global prevalence of dementia, and to global costs (informal care,direct medical and social care costs, and total costs)Proportion of peoplewith dementia0.9%7.9%0.0%0.9%15.5%12.6%7.0%19.6%3.1%5.3%12.3%0.9%0.7%3.3%1.7%3.0%3.2%0.2%1.0%0.3%0.5%100%Informal care(all ADL)1.7%13.7%0.0%0.2%6.1%0.9%0.7%34.6%3.4%3.2%31.3%0.6%0.1%0.6%0.9%0.9%0.8%0.0%0.1%0.2%0.0%100%Direct costsMedicalSocial0.7%2.0%5.4%16.5%0.0%0.0%0.3%0.1%4.5%1.1%1.2%0.2%1.5%0.3%31.3%36.3%2.8%1.1%3.6%1.2%38.2%38.1%0.8%0.3%0.3%0.1%2.7%0.9%1.5%0.5%2.8%0.9%2.1%0.2%0.0%0.0%0.1%0.0%0.1%0.0%0.0%0.0%100%100%Total costs1.7%13.6%0.0%0.2%3.7%0.7%0.7%34.8%2.3%2.4%35.3%0.5%0.2%1.1%0.8%1.2%0.7%0.0%0.1%0.1%0.0%100%
AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
Table 10
Aggregated cost types as percentages of total costs in the different WHO regionsInformal care(all ADL)42.7%42.1%74.7%45.2%68.0%57.1%44.4%41.4%60.5%55.6%37.0%50.3%37.5%24.1%46.6%29.9%42.3%60.0%70.1%75.3%62.8%41.7%Direct costsMedicalSocial7.0%50.3%6.4%51.5%16.9%8.4%29.5%25.2%19.3%12.7%28.7%14.2%37.2%18.4%14.4%44.2%18.8%20.7%23.9%20.5%17.3%45.7%26.1%23.7%32.7%29.7%39.8%36.1%28.0%25.4%36.8%33.4%45.7%12.0%26.8%13.2%20.0%9.9%16.5%8.2%24.9%12.3%16.0%42.3%Total costs100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%100%
AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
Alzheimer’S diSeASe iNTerNATioNAl
26
World Alzheimer reporT 2010
Table 11
Cost per person with dementia in each WHO region (US$)Direct costsInformalcareNon-(all ADL) Medical medicalTotalcosts32370290576059286240789031601301221289176674860590923663553682436881392610811122683496916986
Total costs
AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa WestAll
138121224345261295277451571112479780142611796845701375133538382057166064878751496097084
226218521026845788259595432824231832840323711200220223092529179428922411272412711
1629614963508723517128295133152667157322233215110891999209522954721431115581197191
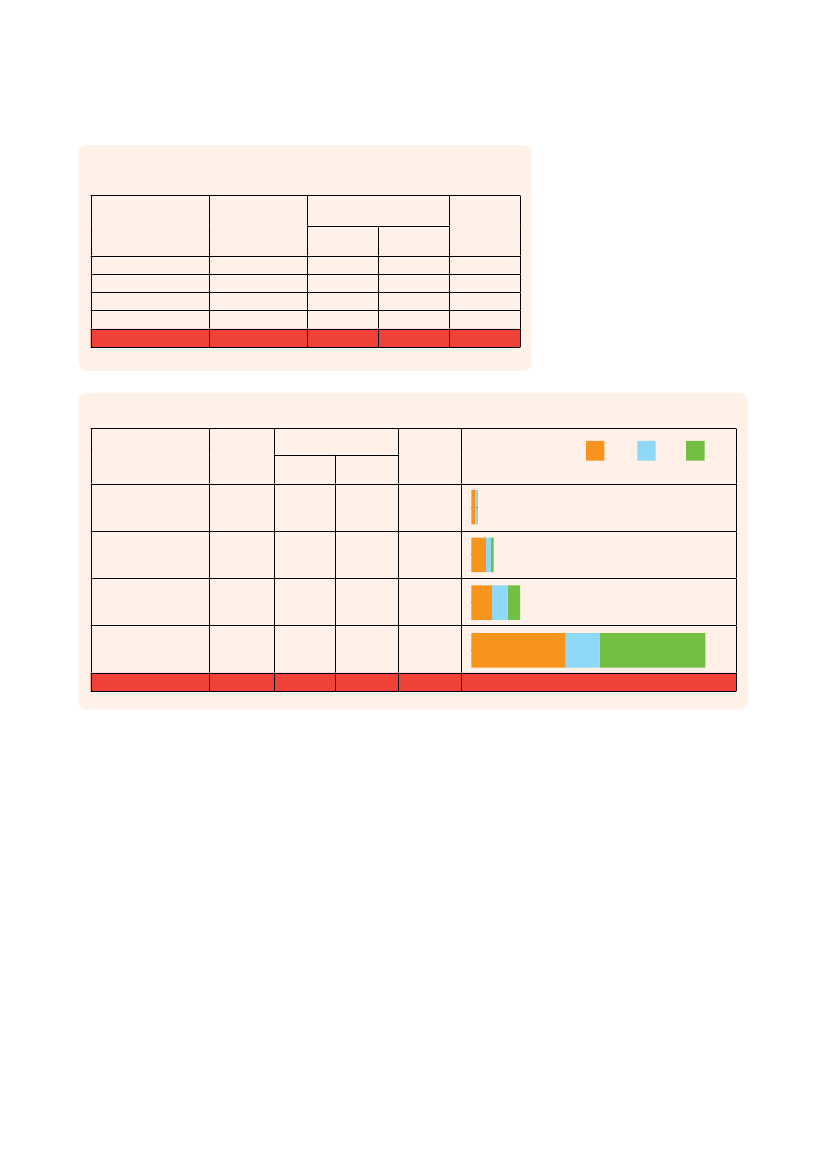
Table 12
Aggregated costs in different World Bank income groups (billions US$)Number ofpeople withdementiaInformalcare(all ADL)2.5218.9013.70216.77251.89
Direct costsMedical1.236.7410.4478.0096.41
Non-medical0.623.578.35243.14255.69
Total costs4.3729.2132.49537.91603.99
Percent ofGDP0.24%0.35%0.50%1.24%1.01%
Low incomeLower middle incomeUpper middle incomeHigh incomeAll
5036979939520447590251636750835558717
Table 13Aggregated costs in different World Bank income groups,as percentages of total global costsPrevalenceLow incomeLower middle incomeUpper middle incomeHigh incomeAll14.2%26.4%13.4%46.0%100%
Informal care(all ADL)1.0%7.5%5.4%86.1%100%
Direct costsMedical1.3%7.0%10.8%80.9%100%
Social0.2%1.4%3.3%95.1%100%
Totalcosts0.7%4.8%5.4%89.1%100%
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
27
Table 14Aggregated cost types as percentages of total costs in different WorldBank income groupsDirect costsMedical28.2%23.1%32.1%14.5%16.0%
Informal care(all ADL)Low incomeLower middle incomeUpper middle incomeHigh incomeAll57.6%64.7%42.2%40.3%41.7%
Social14.3%12.2%25.7%45.2%42.3%
Totalcosts100%100%100%100%100%
Table 15
Costs per person with dementia in different World Bank income groups (US$)Informalcare(all ADL)Direct costsMedical2447172,1944,766
Social1243801,75514,855
Totalcosts8683,1096,82732,865
Care costs
Informal
Medical
Social
Low incomeLower middle incomeUpper middle incomeHigh income
5002,0122,87913,244
All
7,084
2,711
7,191
16,986
Alzheimer’S diSeASe iNTerNATioNAl
28
World Alzheimer reporT 2010
Sensitivity analysesFor the estimation of costs in the base case, wemade several assumptions, regarding, for example,the appropriate method for comparing costsbetween countries, the types of informal care thatshould be included in cost estimations, the hourlycosts to be attached to informal caregiver inputs,Table 16Summary of sensitivity analysis optionsBase case option
and the relative cost of inputs from different typesof caregiver. In order to understand the effect ofthese assumptions on the cost estimations, wecarried out sensitivity analyses in which we variedthese assumptions. The base case options andthe sensitivity analysis options are summarized intable 16.
ConsiderationHow should we compare costs between countries, using a single cost metric?Which informal care inputs should be included?
Sensitivity analysis option(s)According to purchasing power parity (PPP)1 Assistance with basic ADL only2 Assistance with combined ADL and time spentsupervising1 A regression model of average wage as afunction of GDP per person2 At replacement cost (the average wage for asocial care professional)1 Spouse caregiver inputs should be costed at25% of the average wage2 Spouse caregiver inputs should be costed at50% of the average wage
According to the exchangerate with US dollarAssistance with both basicand instrumental ADL (referredto as combined ADL), but nottime spent supervisingAt the average wage for thatcountry based on manualimputationEqually for spouses and non-spouses
How should we cost the inputs of informal caregivers?
How should we compare costs betweencountries, using a single cost metric?There are essentially two approaches: throughexchange rates (as used in the base option) orthrough purchasing power parity (PPP). One USdollar exchanged into Indian rupees and spent inIndia would have more purchasing power in Indiathan it would in the USA. The PPP approach uses aninternational dollar as the standard metric, equalizingthe purchasing power of different currencies for agiven basket of goods.Using a PPP basis is arguably more useful thanexchange rates when comparing generalizeddifferences in living standards between nationsbecause PPP takes into account the relative costof living and the inflation rates of the countries,while exchange rates may distort real differences inincome. For our purposes, the PPP estimates takeinto account the local value of the costs incurred, asopposed to their value on the international moneymarkets. If PPPs are used for the estimates instead
of exchange rates, the total worldwide costs are 7.4%higher. However, PPP is most useful when comparingcosts between countries and regions, particularlythose with widely differing levels of economicdevelopment. In relative terms, the contribution fromlower income countries is more substantial (table 17).Under the base case option, low income countriesaccounted for just 0.7% of total worldwide costs,middle income countries for 10.2% and high incomecountries for 89.1%. Using PPP, these proportionsare 2.1% for low, 20.0% for middle income and 77.9%for high income countries.The costs of dementia as a proportion of GDP arescarcely affected by the choice of exchange rates orPPP-based approaches, since both the numeratorand the denominator are increased in lower incomecountries. Using PPP, this proportion varied from0.25% in low income countries to 0.37% in lowermiddle to 0.54% in upper middle to 1.25% in highincome countries.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
29
Table 17Regions
Sensitivity analysis: Costs estimates based on PPPs (billions US$)Informal care(all ADL)3.9433.000.120.7527.166.953.8976.1012.1113.9278.721.810.872.974.687.073.390.050.791.060.217.7036.1336.47199.24
Direct costsMedical0.715.290.020.489.663.473.1227.033.995.7236.830.910.533.492.262.883.050.030.150.210.093.8614.9018.6672.50
Non-medical5.0842.780.010.415.901.721.5583.694.254.9197.420.830.483.162.052.611.030.020.070.110.041.957.8815.41232.88
Total costsPPPs9.7381.080.151.6442.7112.138.56186.8120.3524.56212.983.551.889.628.9912.567.470.101.021.380.3513.5158.9270.54504.63
Total costs(base case)10.0882.130.100.9422.414.043.97210.1214.1914.33213.042.980.936.565.077.264.500.070.400.690.184.3729.2132.49537.91
AustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa West
Low incomeLower middle incomeUpper middle incomeHigh incomeWorldwide (all)
279.55
109.93
258.12
647.6
603.99
Which informal care inputs should beincluded?For the base case option, we costed time spentby informal caregivers assisting with basic ADL(personal care) and instrumental activities of dailyliving. Inclusion of time spent assisting with IADLmay be problematic given that the ingredients of thiscomponent of care may vary substantially acrosscultures, and that estimates between studies tend tovary substantially depending partly on the methodsused to quantify it. On the other hand, a relativelyhigh proportion of studies included in our systematicreview provided estimates of time spent assistingwith both types of ADL combined. Time spentgenerally supervising the person with dementia iseven more difficult to quantify, and hence estimatesare highly variable. Nevertheless, both IADL
assistance and supervision are generally consideredimportant and time-consuming aspects of informalcare, and a focus on personal care alone is likely toseriously underestimate the extent of informal careinputs and associated costs. Thus, to highlight thecomplexity in caregiving and estimates of caregivertime, we also include basic ADLs (representing aminimum level) and combined ADLs and supervisiontogether (representing a maximum level) as optionsfor the cost estimates of informal care.If only basic ADLs are used for the costs of informalcare instead of combined ADLs (basic ADLs andIADLs), the total costs are 22% lower (table 18)while they are 30% higher if combined ADLs andsupervision are included. Compared with the totalworldwide cost estimate of US$604 billion in thebase case, these sensitivity analyses provide a
Alzheimer’S diSeASe iNTerNATioNAl
30
World Alzheimer reporT 2010
lower bound estimate of US$470 billion (basic ADLsonly) and an upper bound estimate of US$783billion (including assistance with basic ADLs andIADLs, and supervision). The proportions of totalcosts accounted for by informal care are highestin low income and lower middle income countries,particularly in the combined ADLs and supervisionalternative (68-73%).
How should we cost the inputs ofinformal caregivers?Not only the quantification of informal care butalso the costing is crucial for the final estimatedtotal costs. In the approach used in the base case,the inputs of informal caregivers were costed asthe average hourly wage for that country withan adjustment for the difference in the averagewage earning potential of men and women. Theseestimates could therefore be considered to represent
Table 18
Sensitivity analysis
Costs of informal care, and informal care costs as a % of total costs when informal care inputs are considered as a) basic combinedADL and IADL (the base case), b) basic ADL assistance only and c) combined ADL assistance and supervision (billions US$)Base case(combined basic ADLand IADL assistance)Costs ofinformalcare4.3034.600.070.4315.242.311.7787.058.597.9678.761.500.351.582.362.171.900.040.280.520.112.5218.9013.70216.77
Basic ADL assistanceonlyCosts ofinformalcare2.5919.400.060.2011.821.140.8823.193.633.8441.591.500.351.581.562.161.480.020.160.290.061.3013.929.3092.98
Combined ADLassistance andsupervisionCosts ofinformalcare5.8446.160.090.9920.353.622.55162.5115.7314.48135.912.750.664.253.964.385.400.070.460.850.183.9028.0926.27372.93
RegionsAustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa West
% of totalcosts42.7%42.1%74.7%45.2%68.0%57.1%44.4%41.4%60.5%55.6%37.0%50.3%37.5%24.1%46.6%29.9%42.3%60.0%70.1%75.3%62.8%57.6%64.7%42.2%40.3%
% of totalcosts31.0%29.0%70.1%28.0%62.3%39.6%28.5%15.9%39.3%37.6%23.6%50.3%37.5%24.1%36.6%29.8%36.3%45.4%56.5%62.8%48.3%41.2%57.4%33.1%22.5%
% of totalcosts50.3%49.3%78.8%65.6%74.0%67.6%53.6%56.9%73.7%69.5%50.3%65.0%53.1%46.0%59.4%46.3%67.6%71.0%79.3%83.3%73.4%67.8%73.2%58.3%53.7%
Low incomeLower middle incomeUpper middle incomeHigh incomeAll (informal care)All (total costs)
251.89603.99
41.7%
117.50469.60
25.0%
431.20783.29
55.0%
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
31
theoretical lost productivity, assuming that, if theywere not providing informal care for a person withdementia, the caregivers might all form part of thelabour force and contribute to GDP. In the baseoption, imputation for missing data was made fromnearby countries with similar GDP per person andassumed similar care patterns. This approach mayinclude bias. Another option is to make a regressionmodel with average wage as the dependent variableand GDP per person as the explanatory variable.This regression model showed that a change of GDPper person by US$1 will change the hourly averagewage per hour by US$0.000263 (95% confidenceinterval 0.000214-0.000312; p<0.0001, r2=0.48). Ifthis model is applied for missing data (table 19), theresults are very similar to the base option. Data fromTable 19Sensitivity analysis (billions US$)
countries with imputed data represented in mostcases low income countries with relatively smallpopulations of people with dementia.However, a substantial proportion of caregivers arespouses (generally around 40%, but between 15%to 51% by region – see table 7) and most, but not all,could be assumed to be beyond the usual workingage. For the sensitivity analyses, we recalculatedinformal care and total costs valuing the care inputsof spouse caregivers at 50% and 25% of the averagewage, and applying this reduced wage to theestimated proportion of caregivers in each countrythat were spouses. This leads to a reduction in thetotal worldwide cost estimate from US$604 billionin the base case to US$548 billion (a 9% reduction
Total costs using a regression based model for imputation of missing data for costs of informal careRegressionmodel10.0880.780.090.9322.364.033.83210.0014.1914.27213.043.000.936.445.077.244.190.070.260.680.164.1928.8732.20536.38
RegionsAustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa West
Base case10.0882.130.100.9422.414.043.97210.1214.1914.33213.042.980.936.565.077.264.500.070.400.690.184.3729.2132.49537.91
Lower bound of the95% confidenceinterval10.0880.540.090.9322.344.033.80209.9514.1914.25213.042.920.936.425.077.244.110.060.240.680.154.1628.8032.04536.05
Upper bound of the95% confidenceinterval10.0881.030.090.9322.384.033.86210.0514.1914.28213.043.080.936.465.077.254.270.070.280.680.174.2228.9332.35536.71
Low incomeLower middle incomeUpper middle incomeHigh incomeAll
603.99
601.63
601.06
602.21
Alzheimer’S diSeASe iNTerNATioNAl
32
World Alzheimer reporT 2010
when costed at 50% of the average wage) and toUS$520 billion (a 14% reduction when costed at 25%of the average wage).Another way of looking at care inputs is that the valueto society is the same regardless of whether thecare is provided by women or men, or by youngerand potentially economically active or older andretired caregivers. This is the implicit viewpoint whenassessing ‘replacement costs’, namely the cost tosociety of replacing the informal caregiver with a paidsocial care professional. We estimated the averagewage of a social care professional from the Laborsta
database (health and social work)iwhere the averagewage in the health and social sector was availableand applied this to all informal care inputs.
Comparison of this Report withprevious worldwide cost estimates ofdementiaIn 2007, the worldwide costs of dementia wereestimated as US$315 billion(12), later updated toUS$422 billion for 2009(13). The basic assumptionsin these papers were different from those in thisReport. Firstly, only basic ADL assistance rather
Table 20
Sensitivity analysis (billions US$)
Total costs, with the costs of informal care calculated a) with different assumptions regarding hourly wage cost for spouse caregivers,and b) as replacement costsBase case (retiredspouse proportionvalued at 100% ofaverage wage)10.0882.130.100.9422.414.043.97210.1214.1914.33213.042.980.936.565.077.264.500.070.400.690.184.3729.2132.49537.91
RegionsAustralasiaAsia Pacific High IncomeOceaniaAsia CentralAsia EastAsia SouthAsia SoutheastEurope WesternEurope CentralEurope EasternNorth America High IncomeCaribbeanLatin America AndeanLatin America CentralLatin America SouthernLatin America TropicalNorth Africa / Middle EastSub-Saharan Africa CentralSub-Saharan Africa EastSub-Saharan Africa SouthernSub-Saharan Africa West
Spouse caregivingvalued at 50% ofaverage wage9.1575.980.080.8619.373.763.90190.6312.5112.89192.432.840.916.494.526.674.140.060.350.580.154.0425.7330.09488.44
Spouse caregivingvalued at 25% ofaverage wage8.6972.910.080.8217.863.623.86180.8911.6712.17182.132.780.896.454.256.383.950.060.320.530.143.8723.9828.89463.70
Replacement cost(average wagefor a social careprofessional)10.2286.070.060.8217.114.025.02218.1714.5114.92218.813.210.826.834.087.084.020.070.280.440.174.3622.9431.65557.75
Low incomeLower middle incomeUpper middle incomeHigh incomeAll
603.99
548.29
520.44
616.71
i Laborsta Internet [database on the Internet]. ILO. 2010 [cited2010-02-23]. Available from: http://laborsta.ilo.org/STP
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
33
than combined basic ADL and IADL assistance wereincluded in the base option for estimating the costsof informal care, and PPPs instead of exchangerates were used for the currency transformations.The number of basic ADL hours per day was alsosomewhat lower and uniform across the world inthe 2005 and 2009 estimates (1.6 hours per day).However, in the sensitivity analyses for these earlierestimates, options similar to those applied in thecurrent Report were included, making more directcomparisons possible. When doing so, it is clear thatthe costs per person with dementia are very similar,particularly for the combined ADLs (table 21). If theapproach in the 2005 estimates had been used for2010, the cost of illness with combined ADLs wouldactually have been somewhat higher (US$668 billion).However, this figure cannot be interpreted as adecrease in costs; it just highlights methodologicalissues (for the 2010 estimate we have more inputs ofpopulation based data, see comment on page 13).The number of people with dementia increased by18% between 2005 and 2010.
Table 21
Comparisons with current cost estimates and previous reports with similar assumptionsBase caseWimo et al, 20102009US$421.6 billion34,376,044US$645.3 billionUS$447.2 billionUS$18,147US$12,577
Wimo et al, 20072005US$315.4 billion29,336,448US$668.3 billionUS$465.1 billionUS$18,796US$13,079
YearUnadjusted cost of illness estimate in studyNumber of people with dementia as estimated in studyCost of illness including combined (all ADLs) (PPPs,inflated to 2010, prevalence of 2010)*Cost of illness including core (basic) ADLs (PPPs,inflated to 2010), prevalence of 2010)*Total cost per person with dementia including all(combined) ADLs (PPPs, inflated to 2010)*Total cost per person with dementia including core(basic) ADLs (PPPs, inflated to 2010)**costs inflated to 2010 by using average world inflation figures.
2010US$604.0 billion35,558,717US$647.6 billionUS$509.3 billionUS$18,212US$14,322
Alzheimer’S diSeASe iNTerNATioNAl
34
World Alzheimer reporT 2010
references for methods And results1Rice DP, Hodgson TA, Kopstein AN. The economic costsof illness: a replication and update. Health Financing Rev.1985;7:61-80.Lindgren B. Costs of illness in Sweden 1964-1975. Lund:Liber; 1981.Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, HuangY, et al. Contribution of chronic diseases to disability inelderly people in countries with low and middle incomes: a10/66 Dementia Research Group population-based survey.Lancet. 2009 Nov 28;374(9704):1821-30.Sousa RM, Ferri CP, Acosta D, Guerra M, Huang Y, Jacob K,et al. The contribution of chronic diseases to the prevalenceof dependence among older people in Latin America, Chinaand India: a 10/66 Dementia Research Group population-based survey. BMC Geriatr. 2010;10:53.Alzheimer’s Disease International. World Alzheimer Report2009. London: Alzheimer’s Disease International; 2009.Donaldson C, Mugford M, Vale L. Evidence-based healtheconomics. London: BMJ Books; 2002.Drummond MF, O’Brien B, Stoddart GL, Torrance GW.Methods for the economic evaluation of health careprogrammes. Oxford, UK: Oxford University Press; 1997.van den Berg B, Brouwer WB, Koopmanschap MA.Economic valuation of informal care. An overview of methodsand applications. Eur J Health Econ. 2004 Feb;5(1):36-45.Jönsson L. Pharmacoeconomics of cholinesteraseinhibitors in the treatment of Alzheimer´s disease.Pharmacoeconomics. 2003;21:1025-37.21 Allegri RF, Butman J, Arizaga RL, Machnicki G, SerranoC, Taragano FE, et al. Economic impact of dementia indeveloping countries: an evaluation of costs of Alzheimer-type dementia in Argentina. Int Psychogeriatr. 2007Aug;19(4):705-18.22 Scuvee-Moreau J, Kurz X, Dresse A. The economic impactof dementia in Belgium: results of the National DementiaEconomic Study (NADES). Acta Neurol Belg. 2002Sep;102(3):104-13.23 Jönsson L, Berr C. Cost of dementia in Europe. Eur J Neurol.2005 Jun;12 Suppl 1:50-3.24 Kronborg Andersen C, Sogaard J, Hansen E, Kragh-Sorensen A, Hastrup L, Andersen J, et al. The cost ofdementia in Denmark: the Odense Study. Dement GeriatrCogn Disord. 1999;10(4):295-304.25 Jönsson L, Eriksdotter Jönhagen M, Kilander L, SoininenH, Hallikainen M, Waldemar G, et al. Determinants of costsof care for patients with Alzheimer’s disease. Int J GeriatrPsychiatry. 2006 May;21(5):449-59.26 Rigaud AS, Fagnani F, Bayle C, Latour F, Traykov L, ForetteF. Patients with Alzheimer’s disease living at home in France:costs and consequences of the disease. J Geriatr PsychiatryNeurol. 2003 Sep;16(3):140-5.27 Kenigsberg P. Regional patterns – France. Cost of dementia.In: Europe A, editor. European Collaboration on Dementia.Luxembourg: AE; 2009.28 Schulenberg J, Schulenberg I. Cost of treatment and costof care for Alzheimer´s disease in Germany. In: Wimo A,Jönsson B, Karlsson G, Winblad B, editors. The HealthEconomics of dementia. London: John Wiley & Sons.; 1998.p. 217-30.29 O’Shea E, O’Reilly S. The economic and social cost ofdementia in Ireland. Int J Geriatr Psychiatry. 2000;15(3):208-18.30 Beeri MS, Werner P, Adar Z, Davidson M, Noy S. Economiccost of Alzheimer disease in Israel. Alzheimer Dis AssocDisord. 2002 Apr-Jun;16(2):73-80.31 Coduras A, Rabasa I, Frank A, Bermejo-Pareja F, Lopez-Pousa S, Lopez-Arrieta JM, et al. Prospective one-yearcost-of-illness study in a cohort of patients with dementiaof Alzheimer’s disease type in Spain: the ECO study. JAlzheimers Dis. Jan;19(2):601-15.32 Lopez-Bastida J, Serrano-Aguilar P, Perestelo-Perez L,Oliva-Moreno J. Social-economic costs and quality of life ofAlzheimer disease in the Canary Islands, Spain. Neurology.2006 Dec 26;67(12):2186-91.33 Mesterton J, Wimo A, By A, Langworth S, Winblad B,Jönsson L. Cross Sectional Observational Study on theSocietal Costs of Alzheimer’s Disease. Curr Alzheimer Res.2009 Nov 26.34 Wimo A, Johansson L, Jönsson L. Demenssjukdomarnassamhällskostnader och antalet dementa i Sverige 2005 (Thesocietal costs of dementia and the number of dementedin Sweden 2005) (in Swedish). Stockholm: Socialstyrelsen;2007. Report No.: 2007-123-32 .35 Knapp M, Prince M. Dementia UK. London: Alzheimer’sSociety; 2007.36 Luengo-Fernandez R, Leal J, Gray A. Dementia 2010.Oxford: The Health Economics Research Centre, Universityof Oxford; 2010.37 Zencir M, Kuzu N, Beser NG, Ergin A, Catak B, Sahiner T.Cost of Alzheimer’s disease in a developing country setting.Int J Geriatr Psychiatry. 2005 Jul;20(7):616-22.38 Ersek K, Kovacs A, Wimo A, Karpati K, Brodszky V, L J, etal. Costs of dementia in Hungary. Journal of Nutrition, Healthand Aging. 2010:(in press).
23
4
567
8
9
10 Drummond MF, Sculper MJ, Torrance GW, O´Brien BJ,Stoddart GL. Methods for the economic evaluation of healthcare programmes. 3rd ed. Oxford: Oxford University Press;2004.11 Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L,Ganguli M, et al. Global prevalence of dementia: a Delphiconsensus study. Lancet. 2005 Dec 17;366(9503):2112-7.12 Wimo A, Jönsson L, Winblad B. An estimate of the totalworldwide societal costs of dementia in 2005. Alzheimer´sand Dementia. 2007;3:81-91.13 Wimo A, Winblad B, Jönsson L. The worldwide societalcosts of dementia: Estimates for 2009. Alzheimers Dement.2010 Mar;6(2):98-103.14 SBU. Dementia. A systematic review. Stockholm: Statenberedning för medicinsk utvärdering (SBU) (The SwedishCouncil on Technology Assessment in Health Care) 2008.Report No.: 172E/1-3.15 Jönsson L, Wimo A. The cost of dementia in Europe: areview of the evidence, and methodological considerations.Pharmacoeconomics. 2009;27(5):391-403.16 Alzheimer Society. Rising tide:The impact of dementia onCanadian society. Toronto; 2010.17 Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcarecosts and utilization for Medicare beneficiaries withAlzheimer’s. BMC Health Serv Res. 2008;8:108.18 Kuo TC, Zhao Y, Weir S, Kramer MS, Ash AS. Implicationsof comorbidity on costs for patients with Alzheimer disease.Med Care. 2008 Aug;46(8):839-46.19 Zhu CW, Scarmeas N, Torgan R, Albert M, Brandt J,Blacker D, et al. Longitudinal study of effects of patientcharacteristics on direct costs in Alzheimer disease.Neurology. 2006 Sep 26;67(6):998-1005.20 Alzheimer´s Association. 2010 Alzheimer’s disease facts andfigures. Alzheimers Dement. 2010 Mar;6(2):158-94.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
35
39 Goss J. Projection of Australian health care expenditureby disease, 2003 to 2033 Canberra: Australian Institute ofHealth and Welfare; 2008.40 Access Economics Pty Limited. Keeping dementia frontof mind: incidence and prevalence 2009-2050: AccessEconomics Pty Limited; 2009.41 Access Economics PTY Limited. The Dementia Epidemic:Economic Impact And Positive Solutions For Australia.Canberra: Access Economics PTY Limited; 2003.42 AIHW. Dementia in Australia. National data analysis anddevelopment. Canberra: Australian Institute of Health andWelfare.; 2007. Report No.: AIHW Cat. No. AGE 53.43 Acces Economics PTY Limited. Dementia Economic ImpactReport 2008: Access Economics PTY Limited; 2008.44 Wang G, Cheng Q, Zhang S, Bai L, Zeng J, Cui PJ, et al.Economic impact of dementia in developing countries: anevaluation of Alzheimer-type dementia in Shanghai, China. JAlzheimers Dis. 2008 Sep;15(1):109-15.45 Kang IO, Lee SY, Kim SY, Park CY. Economic cost ofdementia patients according to the limitation of the activitiesof daily living in Korea. Int J Geriatr Psychiatry. 2007Jul;22(7):675-81.46 Suh GH, Knapp M, Kang CJ. The economic costs ofdementia in Korea, 2002. Int J Geriatr Psychiatry. 2006Aug;21(8):722-8.47 Almberg B, Grafstrom M, Krichbaum K, Winblad B. Theinterplay of institution and family caregiving: relationsbetween patient hassles, nursing home hassles andcaregivers’ burnout. Int J Geriatr Psychiatry. 2000Oct;15(10):931-9.48 Jansson W, Almberg B, Grafstrom M, Winblad B. The CircleModel–support for relatives of people with dementia. Int JGeriatr Psychiatry. 1998 Oct;13(10):674-81.49 Max W, Webber P, Fox P. Alzheimer’s disease. The unpaidburden of caring. J Aging Health. 1995;7(2):179-99.50 Wimo A, Winblad B, Grafstrom M. The social consequencesfor families with Alzheimer’s disease patients: potentialimpact of new drug treatment. Int J Geriatr Psychiatry. 1999May;14(5):338-47.51 Schulz R, Beach SR. Caregiving as a risk factor for mortality:the Caregiver Health Effects Study. Jama. 1999 Dec15;282(23):2215-9.52 Nordberg G, von Strauss E, Kareholt I, Johansson L, WimoA. The amount of informal and formal care among non-demented and demented elderly persons-results from aSwedish population-based study. Int J Geriatr Psychiatry.2005 Aug 22;20(9):862-71.53 Wimo A, von Strauss E, Nordberg G, Sassi F, Johansson L.Time spent on informal and formal care giving for personswith dementia in Sweden. Health Policy. 2002 Sep;61(3):255-68.54 Langa KM, Chernew ME, Kabeto MU, Herzog AR, OfstedalMB, Willis RJ, et al. National estimates of the quantity andcost of informal caregiving for the elderly with dementia. JGen Intern Med. 2001 Nov;16(11):770-8.55 Moore MJ, Zhu CW, Clipp EC. Informal costs ofdementia care: estimates from the National LongitudinalCaregiver Study. J Gerontol B Psychol Sci Soc Sci. 2001Jul;56(4):S219-28.56 Rice DP, Fox PJ, Max W, Webber PA, Lindeman DA, HauckWW, et al. The economic burden of Alzheimer’s disease care.Health Aff (Millwood). 1993;12(2):164-76.57 Stommel M, Collins CE, Given BA. The costs of familycontributions to the care of persons with dementia.Gerontologist. 1994 Apr;34(2):199-205.
58 Koopmanschap MA. Indirect costs and costing informalcare. In: Wimo A, Karlsson G, Jönsson B, Winblad B, editors.The Health Economics of dementia. London: John Wiley &Sons; 1998. p. 245-56.59 Jönsson B, Jönsson L, Wimo A. Cost of dementia. In: MayM, Sartorius N, editors. Dementia WPA Series Evidence andexperience in Psychiatry. London: John Wiley & Son; 2000. p.335-63.60 van den Berg B, Brouwer W, van Exel J, Koopmanschap M,van den Bos GA, Rutten F. Economic valuation of informalcare: lessons from the application of the opportunity costsand proxy good methods. Soc Sci Med. 2006 Feb;62(4):835-45.61 McDaid D. Estimating the costs of informal care for peoplewith Alzheimer’s disease: methodological and practicalchallenges. Int J Geriatr Psychiatry. 2001 Apr;16(4):400-5.62 Karlsson G, Jönsson B, Wimo A, Winblad B. Methodologicalissues in health economics of dementia. In: Wimo A, JönssonB, Karlsson G, Winblad B, editors. Health economics ofdementia. London, UK: John Wiley & Sons; 1998. p. 161-9.63 Lanska DJ. Time is money–or is it? Estimating the costs ofinformal caregiving. Neurology. 2002 Jun 25;58(12):1718-9.64 Fukami M. Monetary Valuation of Unpaid Work in 1996-Japan. Tokyo: Department of National Accounts, EconomicResearch Institute, Economic Planning Agency; 1998 .65 Johannesson M, Johansson PO, Jönsson B. Economicevaluation of drug therapy: a review of the contingentvaluation method. Pharmacoeconomics. 1992 May;1(5):325-37.66 Gustavsson A, Jönsson L, McShane R, Boada M, Wimo A,Zbrozek AS. Willingness-to-pay for reductions in care need:estimating the value of informal care in Alzheimer’s disease.Int J Geriatr Psychiatry. 2009 Sep 14.67 Matthews FE, Dening T. Prevalence of dementia ininstitutional care. Lancet. 2002 Jul 20;360(9328):225-6.68 Macdonald A, Cooper B. Long-term care and dementiaservices: an impending crisis. Age Ageing. 2007 Jan;36(1):16-22.69 Ostbye T, Crosse E. Net economic costs of dementia inCanada. Cmaj. 1994;151(10):1457-64.70 Feldman H, Gauthier S, Hecker J, Vellas B, Emir B, MasteyV, et al. Efficacy of donepezil on maintenance of activities ofdaily living in patients with moderate to severe Alzheimer’sdisease and the effect on caregiver burden. J Am GeriatrSoc. 2003 Jun;51(6):737-44.71 Gustavsson A, L J, Rapp T, Reynish E, Ousset PJ, Andrieu S,et al. Differences in resource use and costs of dementia carebetween European countries: baseline data from the ICTUSstudy J Nutr Health Aging (in press). 2010.72 Neubauer S, Holle R, Menn P, Grossfeld-Schmitz M, GraeselE. Measurement of informal care time in a study of patientswith dementia. Int Psychogeriatr. 2008 Dec;20(6):1160-76.73 Wang H, Gao T, Wimo A, Yu X. Caregiver time and costof home care for Alzheimer’s disease: a clinic-basedobservational study in Beijing, China. Ageing Int (in press).2010.74 Leon J, Cheng CK, Neumann PJ. Alzheimer’s diseasecare: costs and potential savings. Health Aff (Millwood).1998;17(6):206-16.75 Albert SM, Sano M, Bell K, Merchant C, Small S, Stern Y.Hourly care received by people with Alzheimer’s disease:results from an urban, community survey. Gerontologist.1998;38(6):704-14.
Alzheimer’S diSeASe iNTerNATioNAl
36
World Alzheimer reporT 2010
76 Manton KG, Corder LS, Clark R. Estimates and projections ofdementia-related service expenditures. In: Suzman R, SingerB, Manton KG, editors. Forecasting the health of the oldestold. New York: Springer; 1993. p. 207-38.77 Zhu CW, Scarmeas N, Torgan R, Albert M, Brandt J, BlackerD, et al. Clinical characteristics and longitudinal changes ofinformal cost of Alzheimer’s disease in the community. J AmGeriatr Soc. 2006 Oct;54(10):1596-602.78 Feldman HH, Van Baelen B, Kavanagh SM, Torfs KE.Cognition, function, and caregiving time patterns inpatients with mild-to-moderate Alzheimer disease: a12-month analysis. Alzheimer Dis Assoc Disord. 2005 Jan-Mar;19(1):29-36.79 Hux MJ, O’Brien BJ, Iskedjian M, Goeree R, Gagnon M,Gauthier S. Relation between severity of Alzheimer’s diseaseand costs of caring. Cmaj. 1998;159(5):457-65.80 Zhu CW, Scarmeas N, Torgan R, Albert M, Brandt J, BlackerD, et al. Clinical features associated with costs in early AD:baseline data from the Predictors Study. Neurology. 2006Apr 11;66(7):1021-8.81 Nichols LO, Chang C, Lummus A, Burns R, Martindale-Adams J, Graney MJ, et al. The cost-effectiveness ofa behavior intervention with caregivers of patients withAlzheimer’s disease. J Am Geriatr Soc. 2008 Mar;56(3):413-20.82 Zhu CW, Torgan R, Scarmeas N, Albert M, Brandt J, BlackerD, et al. Home health and informal care utilization and costsover time in Alzheimer’s disease. Home Health Care Serv Q.2008;27(1):1-20.83 Lowin A, Knapp M, McCrone P. Alzheimer’s disease in theUK: comparative evidence on cost of illness and volume ofhealth services research funding. Int J Geriatr Psychiatry.2001 Dec;16(12):1143-8.84 Moraes SR, Silva LS. An evaluation of the burden ofAlzheimer patients on family caregivers. Cad Saude Publica.2009 Aug;25(8):1807-15.85 Souetre EJ, Qing W, Vigoureux I, Dartigues JF, Lozet H,Lacomblez L, et al. Economic analysis of Alzheimer’s diseasein outpatients: impact of symptom severity. Int Psychogeriatr.1995;7(1):115-22.86 Wimo A, von Strauss E, Nordberg G, Sassi F, Johansson L.Time spent on informal and formal care giving for personswith dementia in Sweden. Health Policy. 2002 Sep;61(3):255-68.87 Wimo A, Winblad B, Shah SN, Chin W, Zhang R, McRae T.Impact of donepezil treatment for Alzheimer’s disease oncaregiver time. Curr Med Res Opin. 2004 Aug;20(8):1221-5.88 Wimo A, Nordberg G, Jansson W, Grafstrom M. Assessmentof informal services to demented people with the RUDinstrument. Int J Geriatr Psychiatry. 2000 Oct;15(10):969-71.89 Cavallo MC, Fattore G. The economic and social burden ofAlzheimer disease on families in the Lombardy region of Italy.Alzheimer Dis Assoc Disord. 1997;11(4):184-90.90 Dias A, Samuel R, Patel V, Prince M, Parameshwaran R,Krishnamoorthy ES. The impact associated with caring fora person with dementia: a report from the 10/66 DementiaResearch Group’s Indian network. Int J Geriatr Psychiatry.2004 Feb;19(2):182-4.91 Bruce DG, Paley GA, Nichols P, Roberts D, Underwood PJ,Schaper F. Physical disability contributes to caregiver stressin dementia caregivers. J Gerontol A Biol Sci Med Sci. 2005Mar;60(3):345-9.92 Kumamoto K, Arai Y, Zarit SH. Use of home care serviceseffectively reduces feelings of burden among familycaregivers of disabled elderly in Japan: preliminary results.Int J Geriatr Psychiatry. 2006 Feb;21(2):163-70.
93 Papastavrou E, Kalokerinou A, Papacostas SS, Tsangari H,Sourtzi P. Caring for a relative with dementia: family caregiverburden. J Adv Nurs. 2007 Jun;58(5):446-57.94 Prince M. Care arrangements for people with dementiain developing countries. Int J Geriatr Psychiatry. 2004Feb;19(2):170-7.95 Uwakwe R. Satisfaction with dementia care–giving in Nigeria–apilot investigation. Int J Geriatr Psychiatry. 2006 Mar;21(3):296-7.96 Moise P, Schwarzinger M, Um M-Y, al. e. Dementia care in 9OECD countries. A comparative analysis. Paris: OECD; 2004.Report No.: OECD Health Working Papers No 13.97 Anonymous. Caregiving in the U.S. Executive summary:National Alliance for Caregiving; 2009.98 Raccichini A, Castellani S, Civerchia P, Fioravanti P, ScarpinoO. The caregiver’s burden of Alzheimer patients: differencesbetween live-in and non-live-in. Am J Alzheimers Dis OtherDemen. 2009 Oct-Nov;24(5):377-83.99 Germain S, Adam S, Olivier C, Cash H, Ousset PJ, Andrieu S,et al. Does cognitive impairment influence burden in caregiversof patients with Alzheimer’s disease? J Alzheimers Dis. 2009May;17(1):105-14.100 Serrano-Aguilar PG, Lopez-Bastida J, Yanes-Lopez V. Impacton Health-Related Quality of Life and Perceived Burden ofInformal Caregivers of Individuals with Alzheimer’s Disease.Neuroepidemiology 2006;27:136–42.101 Thomas P, Lalloue F, Preux PM, Hazif-Thomas C, Pariel S,Inscale R, et al. Dementia patients caregivers quality of life: thePIXEL study. Int J Geriatr Psychiatry. 2006 Jan;21(1):50-6.102 Muangpaisan W, Praditsuwan R, Assanasen W, SrinonprasertV, Assantachai P, Intalapaporn S, et al. Caregiver Burden andNeeds of Dementia Caregivers in Thailand: A Cross-SectionalStudy. J Med Assoc Thai. 2010;93(5):601-7.103 Patterson TL, Semple SJ, Shaw WS, Yu E, He Y, Zhang MY,et al. The cultural context of caregiving: a comparison ofAlzheimer’s caregivers in Shanghai, China and San Diego,California. Psychol Med. 1998 Sep;28(5):1071-84.104 Liu Z, Albanese E, Li S, Huang Y, Ferri CP, Yan F, et al. Chronicdisease prevalence and care among the elderly in urban andrural Beijing, China – a 10/66 Dementia Research Group cross-sectional survey. BMC Public Health. 2009;9:394.105 Golimbet V, Trubnikov V. Evaluation of the dementia carerssituation in Russia. Int J Geriatr Psychiatry. 2001 Jan;16(1):94-9.106 Svetlana IG, Cleusa PF, Natalya M, Olga S, Sube B, Martin P.Helping carers to care - The 10/66 dementia research group’srandomized control trial of a caregiver intervention in Russia.International Journal of Geriatric Psychiatry. 2009;24(4):347-54.107 Nurock S, Wojciechowska M. What real outcomes matter tocaregivers? Int Psychogeriatr. 2007 Jun;19(3):355-62.108 Demensförbundet. Sammanställning av Demensförbundetsanhörigenkät. Stockholm: Demensförbundet; 2003.109 Souetre E, Thwaites RM, Yeardley HL. Economic impact ofAlzheimer’s disease in the United Kingdom. Cost of careand disease severity for non-institutionalised patients withAlzheimer’s disease. Br J Psychiatry. 1999;174:51-5.110 Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P,et al. Determinants of burden in those who care for someonewith dementia. Int J Geriatr Psychiatry. 2008 Oct;23(10):1078-85.111 Chiu L, Tang KY, Liu YH, Shyu WC, Chang TP. Costcomparisons between family-based care and nursing homecare for dementia. J Adv Nurs. 1999;29(4):1005-12.112 Błedowski P, Pedich W. Eurofamcare: National Background��Report for Poland. Białystok: Warsaw School of Economicsand The Medical University of Białystok, Poland; 2004 July,2004.
Alzheimer’S diSeASe iNTerNATioNAl
37
World Alzheimer report 2010
conclusions andrecommendations
As her cognitive difficulties increase, maria is finding it more difficultto continue to live in her small home in the Villa Francisca barrio inSanto domingo, dominican republic. She is coming to realise thenecessity of moving to a rural area where she has family, but theidea of moving is painful.
Alzheimer’S diSeASe iNTerNATioNAl
38
World Alzheimer reporT 2010
conclusions and recommendationsThe estimated annual worldwide cost to society ofdementia, US$604 billion, highlights the enormousimpact that dementia has on socio-economicconditions worldwide. It is difficult to envisage solarge a sum, but it amounts to around 1% of theworld’s gross domestic product. If dementia carewere a country, it would be the world’s 18th largesteconomy, ranking between Turkey and Indonesia(figure 4)i. If it was a company, it would be the world’slargest by annual revenue exceeding Wal-Mart(US$414 billion) and Exxon Mobil (US$311 billion)ii.The scale of these costs is explainable when oneconsiders that, according to our estimates in theWorld Alzheimer Report 2009, 35.6 million olderpeople worldwide (around 0.5% of the world’s totalpopulation) live with dementia. A high proportionof people with dementia need some care, rangingfrom support with instrumental activities of dailyliving (such as cooking or shopping), to full personalcare and round the clock supervision. In some highincome countries, between one third and one half ofall people with dementia live in resource- and cost-intensive residential or nursing home care facilities.Medical care costs also tend to be relatively high forpeople with dementia, particularly in high incomecountries with reasonable provision of specialist careservices(1). In many such studies, the greater numberof comorbid medical conditions accounts for thehigher use of medical care resources by people withdementia.It is very difficult to make an accurate projection offuture costs, since there are so many things that aredifficult to predict. Future costs could be influencedby macroeconomic factors (for example, the paceof economic development) and by dementia-specific factors. These would include changes in theincidence and prevalence of dementia, in patterns ofhelp seeking, in the availability of health and socialcare services, and changes in care systems and careconditions. The availability of new and more effectivetreatments for dementia might on the one handincrease medical care costs, but on the other reducethe needs for social care. However, if we assume thatall potential background factors remain unchanged,and we factor in only the increases in the number ofpeople with dementia forecast in last year’s WorldAlzheimer Report, then by 2030 worldwide societalcosts will have increased by 85%.
Strengths and weaknessesThe accuracy of any estimate of the worldwide costsof dementia depends critically upon the quality of thedata used to estimate it. These comprise:• The prevalence of dementia.• The resources used with respect to direct medicalcare, social care and informal care.• The costs attached to the resources used.Ideally, these data should be up to date, available forall countries worldwide, and in appropriately fine-grained detail.This Report is based on much better underlyingsources than previous worldwide cost estimates.Estimates of the prevalence and numbers of peoplewith dementia were obtained from the WorldAlzheimer Report 2009, following a fully systematicreview of the literature from around the world. Thereview identified 135 publications, with a largerecent increase in the prevalence survey evidence-base covering low and middle income countries.However, a relatively high proportion of studieswere conducted more than 10 years previously,particularly those from high income countries. Themethodological quality of many studies also leftmuch to be desired. Only in two countries, the USAand Canada, had nationally representative surveysbeen conducted.Data on resource utilization is also more extensivethan previously available, particularly with respectto informal care provision in low and middle incomecountries. The 10/66 Dementia Research Groupstudies in Latin America, India and China provide
Figure 4
Cost of dementia compared to national economies
US$ billions150012009006003000adaiaiamBelgiuoxiceyIndonesSwedeCanmentMeTurkn
i World Bank - Gross domestic product 2009 http://siteresources.worldbank.org/DATASTATISTICS/Resources/GDP.pdfii Wikipedia – list of companies by revenue http://en.wikipedia.org/wiki/List_of_companies_by_revenue
Cost of dementia compared to national economies
Alzheimer’S diSeASe iNTerNATioNAl
De
The GloBAl eCoNomiC impACT oF demeNTiA
39
recent estimates of caregiver characteristics, andof average time spent assisting with basic activitiesof daily living (ADLs) and instrumental activities ofdaily living (IADLs), and time spent supervising,all from representative population-based samplesof people with dementia. This adds significantlyto the pre-existing database generated from asystematic review of 53 economic studies of formaland informal care, which was heavily skewed toEuropean and North American studies. Basedon our comprehensive review of the internationalliterature, we identified estimates of assistance withbasic ADLs for 25 countries, representing 63% ofthe worldwide dementia population, and data onassistance with combined ADLs from 30 countriesrepresenting 73% of the worldwide dementiapopulation. Data on supervision were available for25 countries representing 63% of the worldwidedementia population. For other countries it wasnecessary to make imputations based on availablefigures from nearby countries or in some cases fromregional or global estimates. The regression-basedimputation models showed similar results. However,although this Report is based on better data thanprevious reports, it is important to acknowledgethe limitations with the current evidence base. Themajority of resource utilization studies have beencarried out on ‘convenience samples’ of those whohave accessed services or contacted Alzheimerassociations, and are hence skewed towards thosewith more advanced disease and greater needs forcare, which may result in an overestimate of costs.Generalizing from one sample, in one treatmentfacility, usually in a major city, to the populationof the country as a whole is clearly problematic.Sample sizes are often small, and often based onurban areas, leading to imprecise estimates. Manyof the studies are not recent and since care patternsand care systems change, there is a need for acontinuous update of such figures.The most significant limitation is in the estimation ofdirect costs of both medical and social care. In thisstudy, these figures are partly based on imputationfrom nearby countries but also estimated with aregression model, mainly based on high incomecountries, although cost figures from Turkey,China, Argentina and Hungary are available. Evenif the estimates of direct costs and the distributionbetween direct medical and non-medical costs arethe best possible, these figures must be interpretedwith caution. While estimates of use of medicalcare services from the 10/66 Dementia Research
Group studies in Latin America, India and Chinaadd significantly to our understanding of resourceutilization in this domain, we considered that theglobal coverage of such data was still insufficientto replace the imputed approach. It is particularlyimportant that medical and social care utilizationdata is up to date and locally relevant in order toreflect:• Cultural differences in help-seeking.• National differences in health and social caresystems.• Secular changes in patterns of help-seekinglinked to changes in awareness, availability ofspecific services, promotion of early diagnosis,and access to benefits linked to diagnosis.The results from the ADI worldwide survey of keyinformants regarding placement in residential careis also a great advance from previous studies. Thesurvey showed that there are differences betweenrural and urban areas as well as between high andlow income countries.A general limitation is that our global cost of illnessestimates rely on studies of dementia prevalenceand dementia-related resource utilization that areunequally distributed worldwide, with data lackingfrom many countries. There is a particular lack ofrelevant studies from the continent of Africa, theMiddle East, and from Eastern Europe. The extensivesensitivity analysis we have conducted indicates thedegree of uncertainty in the cost estimates, and weconsequently use the concept of ‘cost estimates’rather than ‘cost calculations’.The sensitivity analysis also reflects the fact thatthere are different opinions of what should beincluded in the cost estimates, particularly regardinginformal care, and how these should be costed.The several presentations in the sensitivity analysisfacilitate comparisons with other studies andapproaches.
The regional distribution of global costsWe have estimated that 89% of total global societalcosts of dementia are incurred in high incomecountries, 10% in middle income countries, andless than 1% in low income countries. However, theminority (46%) of people with dementia live in highincome countries, 39% in middle income, and 14%in low income countries. There is therefore a clearinequity in the global distribution of morbidity andattendant costs, which requires explanation.
Alzheimer’S diSeASe iNTerNATioNAl
40
World Alzheimer reporT 2010
The use of exchange rates to provide a standardmetric for comparing costs across countriesmay have underestimated costs in lower incomecountries, relative to higher income countries. Whenthe PPP approach is used instead, 78% of totalglobal costs are incurred in high income countries,20% in middle income and 2% in low incomecountries.In low and middle income countries (LMIC), informalcare costs predominate (accounting for around twothirds of all costs, compared with around 40% in highincome countries), whereas in high income countries(HIC), direct social care costs account for nearlyhalf of all costs, compared with only one tenth inlower income countries. Since average wages (usedto estimate informal care costs) are much lower inLMIC, this has an important impact on comparativetotal costs. Also, direct social care costs generallyexceed those of informal care, because of the fixedstructural costs involved in employing and managingcommunity social care staff, and maintainingresidential care premises. For example, in the recentDementia UK report(2), while the average annual costper person with dementia was £25,472, costs rangedfrom £14,540 for somebody with mild dementia livingin the community to £20,355 for moderately severedementia living in the community to £31,263 per yearfor those living in care homes.There are surprisingly few reliable estimates of theproportions of people with dementia living in carehomes, and none at all from low and middle incomecountries. In the five regional centres surveyedin the early 1990s for the UK Medical ResearchCouncil Cognitive Function and Ageing Study, 34%(95% confidence interval 30%-39%) of peoplewith dementia lived in care homes(3). This figureis very close to the 37% that was subsequentlyestimated for the UK as a whole in the DementiaUK report(2). However, another recent estimate fromthe UK, based upon care home market survey datasuggested that as many as 54% of all those withdementia resided in care homes(4). This secondfigure is very close to that estimated in the CanadianStudy of Health and Ageing(5), which is, to date, theonly nationally representative survey of dementia tohave sampled separately private households andinstitutional care settings. In the Dementia UK report,the proportion of those with dementia living in carehomes rose with age, from 27% of those aged 65-74,to 28% of those aged 75-84, to 41% of those aged85-89, to 61% of those aged 90 and over(2). This isunderstandable in the context of the greater severity
of dementia among the oldest old, and the relativepaucity of informal support among older people, whoare more likely to have been widowed and to havelost many of their friends through bereavement.In our analyses, the extent of informal care mayhave been overestimated in HIC relative to LMIC,since most HIC estimates in our database derivedfrom convenience rather than representativepopulation-based studies, which, as we have seen,are likely to be biased towards the inclusion of moreadvanced cases, needing more care. Conversely,the LMIC estimates were based largely on the 10/66population-based studies in Latin America, India andChina. In most 10/66 study sites, between 30% and50% of those with dementia were rated as needing‘no care’. Only 30% of those with mild dementiawere rated as needing ‘much care’, compared with69% of those with moderate dementia, and 88% ofthose with severe dementia. Needs for care wereless evident in rural sites in Latin America and China,and in India, where traditional extended family livingcircumstances still prevailed. In those settings,most older people lived with and were materiallysupported by their children. Instrumental activities ofdaily living (cooking, shopping, cleaning, managingFigure 5The prevalence of needs for care among peoplewith dementia, by research site and severity of dementia(10/66 Dementia Research Group population-based studies,data release 2.2)% needing careMuch careCubaDRPeru UPeru RVenezuelaMexico UMexico RChina UChina RIndia UIndia RMildModerateSevere020406080100Some care
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
41
household budgets) would not be part of the normalroles and responsibilities even of fit and healthy olderadults, who to that extent were ‘cared for’ by theirchildren. Under such circumstances, dependence,beyond cultural norms, might only become apparentwith more advanced dementia(6).These observations regarding possible explanationsfor the inequitable distribution in dementia costsbetween world regions have important implicationsfor future trends. These will inevitably tend towardsmore rapidly increasing per capita and populationcosts in LMIC, in such a way that the globaldistribution of costs will come to resemble that ofmorbidity. Cost increases in LMIC are likely to bedriven by several underlying factors:1 Increases in numbers of people with dementiawill occur much more rapidly in low and middleincome countries, because of the more rapid paceof demographic ageing in those regions. Thus, in theWorld Alzheimer Report 2009, we forecast a 40%increase in numbers in Europe over the 20 years from2010 to 2030, a 63% increase in North America, 77%in the southern Latin American cone, and 89% in thedeveloped Asia Pacific countries(7). These figures formore developed regions are to be compared with117% growth in east Asia, 107% in south Asia, 134-146% in the rest of Latin America, and 125% in northAfrica and the middle East.2 With economic development, average wages,used here to calculate the opportunity costor replacement cost of informal care, will riseparticularly rapidly in low and middle incomecountries.3 If costs can be seen as a proxy for availableresources, it is obvious that resources for dementiacare, particularly formal medical and social care,are unequally distributed worldwide. With increasedawareness will come increased demand for, andsupply of such care.Health care expenditure is lower than it should bein all world regions. Evidence-based interventions,including caregiver support and training, and respitecare should be being routinely provided, but are not,even in high income countries(8). There are very fewestimates of the extent of the ‘treatment gap’ fordementia in LMIC, but it is likely to be much greaterthan in better resourced settings; fewer than 10%of recruits to a widely advertised trial of a caregiverintervention in Goa, south India, had receivedany prior medical attention(9). The World Health
Organization’s Mental Health Gap Action Plan aimsexplicitly to close this gap in LMIC by boosting thecoverage of evidence-based ‘packages of care’(10)delivered in a cost-effective manner by non-specialisthealth workers in general healthcare settings. Theguidelines (including recommendations for dementiacase finding, diagnosis, caregiver education, trainingand support, and cognitive stimulation for peoplewith dementia) are due to be piloted and evaluated inthe context of scaling up in up to 12 target LMIC from2011. This initiative, if successful, could bring abouta step change in patterns of medical care utilizationin resource poor countries. The cost of suchinterventions, which rely mainly on human resources,will vary between countries according to their wagelevels. However, the cost of drugs that are still onpatent tend to be quite similar worldwide (as wasrecently reported for acetylcholinesterase inhibitorsfor Alzheimer’s disease(11)), and hence relativelyunaffordable in low and middle income countries.Alzheimer’s is currently a very active field for drugdevelopment(12). Any new disease-modifying agentwould have a huge potential market in LMIC, raisingimportant ethical and practical challenges, arguablymeriting a global response on the scale of the GlobalFund and PEPFAR initiatives for HIV/AIDS.Residential care and community social care systems(home care) are well developed in many high incomecountries, but scarce in low and middle incomecountries where there is still a strong reliance ontraditional, informal family care arrangements.However, it seems likely that the need for high qualitycommunity and residential care will grow in LMIC,and with it the direct costs of dementia care. This hascertainly been the case in HIC such as the UnitedKingdom and the USA, which were among thefirst to experience the dementia epidemic. In manydeveloping countries traditional family and kinshipstructures are under threat from the demographic,social and economic changes that accompanyeconomic development and globalisation(13). First,the education of women and their increasingparticipation in the workforce (generally seen aspositive human development indicators), tend toreduce their availability for caregiving and theirwillingness to take on this additional role. Second,populations are increasingly mobile as education,cheap travel and flexible labour markets inducechildren to migrate to cities and abroad to seekwork. Finally, declining fertility in the last stage of thedemographic transition leaves increasing numbers ofolder people, particularly those with no son, lacking
Alzheimer’S diSeASe iNTerNATioNAl
42
World Alzheimer reporT 2010
family support. Its effects will be most evident inChina, where the baby boom encouraged by Maowas sharply reversed by the introduction of the one-child family law in 1978. Over the next twenty years,the parents of these only children will be reaching oldage, and the period of greater risk for dementia anddependence.Some governments in low and middle incomecountries have sought to encourage or coercefamilies to shoulder their responsibility for thefinancial support and care for older parents(14). Forexample, the Indian parliament passed a law in 2007requiring children to support their parents, with thosewho fail to do so facing a three-month prison termwith no right of appeal. The Social Justice Minister,Meira Kumar was quoted as saying:‘This bill is in response to the concerns expressed bymany members over the fate of the elderly. With thejoint family system withering away, the elderly are beingabandoned. This has been done deliberately as they(the children) have a lot of resources which the oldpeople do not have.’
lawmakers, they seem destined to fail in the longer-term. Care homes are already proliferating in majorcities in countries such as India and China, cateringto the affluent middle classes. In Beijing, the 10/66Dementia Research Group survey highlighted thatmore than half of those with dementia were beingcared for, at least in part, by paid caregivers. Thisis largely a by-product of economic development:when urban salaries exceed the cost of purchasingcare by an adequate margin, then families are likelyto opt for this rather than giving up work to care. InJapan, a high income country with a similarly strongConfucian tradition of honouring and caring for theelderly, the government felt obliged, on 1st April2000, to implement a long-term care insurance planentitling those eligible to services worth 365,400yen per month (US$3,840), with the obligation of a10% co-payment(15). Despite initial public misgivingsregarding its cultural appropriateness(15), the newsystem has proved popular with families and care-providing entrepreneurs alike(16), and has beenhelpful in alleviating caregiver strain(17).
The legislation also provides for the state to set upold age homes that the minister said should be the‘last resort for the poor and the childless’. Whilesuch policies are understandable in the contextof the very real social problem identified by Indian
Comparisons with other estimates ofthe cost of dementiaThe previously estimated worldwide CoI of dementia– US$315 billion for 2005(18)and US$422 billion for2009(19)may at a first glance be significantly lowerthan the cost figure in the current paper, US$604billion. However, our sensitivity analyses (table 20,page 32) showed that the differences were mainlyaccounted for by the exclusion of assistance withIADLs from the computation of informal care inputs,and by the increases in numbers of people withdementia over time.There are also some previous aggregated costsestimates for Europe. In the EuroCoDe project(20),the estimated cost of dementia in the EuropeanUnion (EU27) was €160.3 billion in 2008 or €22,194per person with dementia, which corresponds toUS$225.9 billion/US$31,281 in 2008 and US$228.5billion/US$31,633 if inflated to 2010. If we extract thecost figures for EU27 from our current study, theseare slightly lower – US$212.3 billion or US$27,698 perperson with dementia(20). The cost estimates fromthe European Brain Council (EBC) are considerablylower than other estimates.In table 22 we have summarised annual per personcosts derived from previously published cost ofillness studies in different countries and worldregions. All costs are expressed in US dollars,
Table 22Annual costs per person with dementiaderived from previously published cost of illness studies(figures recalculated when necessary to facilitate directcomparison)Costs perperson withdementia (US$– all inflated to2010)60,09049,41334,55231,93930,81230,80525,22224,85024,54416,5854,0123,3932,641
ProjectUSA (21)Sweden (22)Australia (23)EuroCoDe for EU27 (20)Canada (24)UK (2)EuroCoDe for the whole of Europe (20)DWCD for Europe (18;19;25)Hungary (26)European Brain Council project (27)Argentina (28)Turkey (29)China (30)
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
43
and have been inflated to 2010 to facilitate directcomparison. Nevertheless, different studies haveused different sources of information for their costestimates and applied different assumptions. Thiswill account for some of the observed variation.However, it is obvious that the largest singledeterminant of the scale of the costs is the level ofeconomic development of the country or regionconcerned. The per person annual costs in table 22are in general quite consistent with those estimatedin our current report – US$868 in low incomecountries, US$3,109 in low middle income countries,US$6,827 in upper middle income countries andUS$32,865 in high income countries.
states: first, that societal costs are very high, andsecond that the costs of long-term residential careare prominent.There are several CoI studies from the US with agreat range in the cost estimates, illustrating perhapsthe heterogeneity of dementia care in the US butalso heterogeneity in study populations and costingmethods. The Alzheimer’s Association estimatedin their 2010 Alzheimer’s Disease Facts & Figuresreport(21)that the total direct costs of Alzheimer’sdisease and other dementias were US$172 billionin 2010 and the costs of informal care were US$144billion (2009), resulting in a total societal cost ofUS$316 billion. The Alzheimer Society of Canadahas estimated a total national societal cost of 14.9billion Canadian Dollars (US$14.1 billion) for 2008,arising from 481,000 people with dementia, with atenfold increase, to 153 billion over the thirty years to2038(24).From Australia, there are three reports with divergingcost estimates; two studies(32,23)showed similarresults, while a report from Australian Institute ofHealth and Welfare(33), computed significantly lowercosts, based upon a smaller estimated numberof people with dementia, and using a net costsapproach.Very little detailed work has been done on evaluatingthe economic costs of dementia in low or middleincome countries. There are several reasons for this,including a shortage of trained health economists,the low priority given to dementia, and the poorlydeveloped state of services for people withdementia. However, the fundamental obstacle hasbeen the absence of available data sets(34). Giventhat the needs of frail older people will soon cometo dominate health and social care budgets in theseregions, more data is needed, urgently. In Denizli,Turkey a cost analysis was carried out on 42 patientswith dementia(29). In Turkey, only 1% of older peoplelive in residential care, so families provide most ofthe care. The average annual cost of care (excludinghospitalisation) was US$1,766 for mild dementia andUS$4,930 for severe dementia. While most costsincreased with the severity of the disease, out-patientcosts declined. In Argentina(28), the annual directcosts of the disease increased with disease severity,from US$3,420 in mild to US$9,658 in severeAlzheimer’s disease, and with institutionalisation(US$3,189 for community dwelling and US$14,448 forinstitutionalised). Most direct costs were paid for bythe family.
There have been many studies of the cost ofdementia in high income countries. In the UnitedKingdom, the results of an economic analysiscommissioned by the Alzheimer’s Society for theDementia UK report indicated a total annual costof £17 billion in 2005(2)(US$25.5 billion), updatedby the Alzheimer Research Trust to £19.7 billion(US$29.6 billion) for 2010(31). Informal care accountedfor just over one third of the total. The single largestcost driver was the cost of institutional care in carehomes (contributing 41% of the total costs). The costof social care (community care plus care homes)dominates direct costs, accounting for 56% of totalcosts, while health service costs accounted for only8% of the total. In high income countries, coststend to rise as dementia progresses. When peoplewith dementia are cared for at home, informal carecosts may exceed direct formal care costs. As thedisease progresses, and the need for professionalcaregivers and specialist medical care arises, sothe direct social and health care costs will increase.Thus, in the Dementia UK report, while the averageannual cost per person with dementia was estimatedas £25,472 (US$38,208), this varied from £14,540(US$21,810) for a person with mild dementia livingin the community (where informal care makesthe largest contribution) to £20,355 (US$30,534)for a person with moderate dementia living in thecommunity, to £31,263 (US$46,895) for a person withdementia living in a care home(2).Similarly, in a Swedish CoI study(22)the costs ofresidence in care homes constituted about two-thirds of the societal costs, estimated as SEK 50billion in 2005 (US$7.0 billion in 2010) or US$49,413per person per year. The cost estimates from the UKand Sweden illustrate two patterns from ‘welfare’
Alzheimer’S diSeASe iNTerNATioNAl
44
World Alzheimer reporT 2010
In a study from China(30), costs from 67 people withAlzheimer’s disease were collected. Direct costsconstituted US$1,068 (44%) and costs of informalcare US$1,326 (56%) with increasing costs due toseverity. In another study from China(35), amountand costs of informal care in terms of basic ADLs,instrumental ADLs (IADLs) and supervision wasmeasured in 71 people with dementia using theRUD instrument(36). Cost in terms of IADL was thebiggest proportion (US$4,111 per year) followed bysupervision (US$2,841 per year) and basic ADLs(US$2,723 per year).There are also very few studies from Eastern andCentral Europe. ICTUS is a clinical based projectand includes several European countries, includingRomania(37). There is a range in annual costs perperson with dementia (2006 cost level) between€6,063 (Northern Europe) and €8,279 (WesternEurope). As part of the EuroCoDe project(20)aseparate report from Hungary(26)included resourceutilization and cost data on 74 people with mildcognitive impairment or dementia, ranging from €358per month (MCI) to €885 (severe dementia). In boththe ICTUS and Hungarian project, the RUD (resourceutilization dementia) instrument(36)was used for datacollection.
than on cancer research. £590 million was spenton cancer research each year, while £50 millionwas invested in dementia research. Heart diseasereceived £169 million per year and stroke research£23 million. Clearly, investment in research did notmatch the relative burden of these different chronicdiseases. In fact, for every £1 million in care costsarising from the disease(31):––––£129,269 was spent on cancer research.£73,153 on heart disease research.£8,745 on stroke research.£4,882 on dementia research.
In a paper from Sweden(22), the costs of dementiawere compared with other estimates for chronicdisorders. The annual costs of dementia (50 billionSEK) was higher than for depression (32.5 billionSEK), stroke (12.5 billion SEK), alcohol abuse (21-30billion SEK) and osteoporosis (4.6 billion SEK), butthe distribution between the diseases and the typesof costs differ. While, for example, the direct costs ofsocial care constituted the greatest cost componentin dementia, indirect costs in terms of productionlosses dominated for depression.The World Alzheimer Report 2009 highlighted thediscrepancies in the burden arising from differentchronic diseases, depending upon whether rankingis determined according to their contributions todisability or mortality(7). The diseases that contributemost to years lived with disability (dementia, arthritis,stroke and sensory impairments) contribute leastto mortality (where the effects of cardiovasculardisease and cancer predominate), and vice versa.Recently published findings from the 10/66 DementiaResearch Group show clearly that dementia isthe leading chronic disease contributor to bothdisability(38)and needs for care(39). However, mostanalyses of the way that chronic diseases areprioritised suggest that for clinicians, policymakersand researchers what matters most is the quantityrather than the quality of life. In the USA also, theNational Institutes of Health spend 14 times more onresearch into cancer, and five times more is spenton research into cardiovascular disease, than isspent on research into dementiai. Worldwide, in thelast 10 years, there were 16 times as many researchpublications on cancer, and 11 times as many onheart disease(7). Health care expenditure is alsoskewed towards cancer and heart disease.i National Institutes of Health Estimates of Funding for VariousResearch, Condition, and Disease Categories (RCDC)http://report.nih.gov/rcdc/categories/
Comparison with the cost of otherchronic diseasesIt is difficult to compare our estimates of the globalsocietal costs for dementia with those for otherconditions, because few such estimates exist, andthere are problems with comparability in the way thatsocietal costs were computed.In some countries, attempts have beenmade to study this issue, using data that aremore comparable. In the UK, a recent reportcommissioned by the Alzheimer’s Research Trust(Dementia 2010) focused upon the economic burdenof dementia and other chronic diseases, and soughtto compare like-for-like disease costs with nationalexpenditure on research(31). The report’s authorsestimated the annual societal cost of dementia at£23 billion, £12 billion for cancer, £8 billion for heartdisease, and £5 billion for stroke. The societal costsof dementia almost matched those of cancer, heartdisease and stroke combined(31). The annual percapita costs were estimated at £27,647 for dementia,£5,999 for cancer, £4,770 for stroke and £3,455 forheart disease. However, Government and charitablespending on dementia research was 12 times lower
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
45
Alzheimer’s Disease International’s recommendationsGlobally, dementia costs around 1% of GDP, this figure varying between around 0.24% in lowincome countries and 1.24% in high income countries. While the health care costs for dementiaare currently comparatively modest, these are more than made up for by the very high costs ofinformal care (unpaid care provided by families), community social care and, in some developedcountries, residential care homes.In high income countries (for example the United Kingdom, where such a comparison was recentlypublished(31)) it is likely that the societal costs of dementia already exceed those of other chronicconditions such as cancer, heart disease or stroke that are accorded relatively greater priority.The relatively low medical care costs for dementia are explained first by low levels of awarenessand help-seeking. Raising awareness and the promotion of early diagnosis is now a key priority,and countries such as the UK, France and Australia are focusing on this as part of their nationaldementia strategies. However, this is a particular problem for low and middle income countries,where resources for specialist care are also very limited.There is also evidence to suggest that dementia is currently under treated, even in high incomecountries(8). While the efforts of the WHO to increase the coverage of basic packages of care willfocus on non-specialists in resource poor settings, the evidence-based dementia care guidelinesare equally applicable to high income countries, where, for example, few caregivers receiveeducation, training and support(8).Many governments already commit funds for dementia care, but lack strategic awareness of it andof the hidden costs and the pressure that dementia puts on health systems. Currently there arenational plans to improve dementia care in only a few countries. There is no strategy to deal withincreases in the future, which current health systems are not equipped to deal with.1 alzheimer’s disease international calls on all governments to make dementia a healthpriority and develop national plans to alleviate the burden of the disease.2 alzheimer’s disease international reminds governments of their obligations under the unConvention on the Rights of People with disabilities, and the madrid international Plan foraction on ageing to ensure access to healthcare. it calls on governments to fund and expandthe implementation of the WhO mental health Gap action Plan, including the packages of carefor dementia, as one of the seven core disorders identified in the plan.3 alzheimer’s disease international requests that new investment in chronic disease careshould always include attention to dementia. for example, the WhO Global Report on‘innovative Care for Chronic Conditions’(40)alerts policymakers, particularly those in low andmiddle income countries, to the implications of the decreases in communicable diseases andthe rapid ageing of populations. healthcare is currently organized around an acute, episodicmodel of care that no longer meets the needs of patients with chronic conditions. the WhOinnovative Care for Chronic Conditions framework(41)provides a basis on which to redesignhealth systems that are fit for their purpose.Medical care costs remain low because there are currently no pharmacological treatments thathave proven to be effective in preventing or modifying the course of the disease. In addition,psychosocial interventions are also greatly under-researched, and they are under-promoted whenfound to be effective.4 alzheimer’s disease international calls on governments and other major research fundersto act now to increase funding for research into prevention treatment and care. to a levelmore proportionate to the economic burden of dementia. Recently published data from theuK(31)suggests that a 15-fold increase would be required to reach parity with research intoheart disease, and a 30-fold increase to achieve parity with cancer research. internationalcoordination of research is needed to make the best use of resources.
Alzheimer’S diSeASe iNTerNATioNAl
46
World Alzheimer reporT 2010
The costs of chronic diseases to society are driven mainly by long-term disability and dependence,and the resulting costs of social care. Currently, these are largely met by unpaid family caregivers.While governments may regard family care as ‘free’, they do so at their peril. The major driver ofthe need for formal community and residential care (counted as direct social care costs in thisReport) is likely to be the dependency ratio, defined as the number of dependent people dividedby the size of the working age population. Declining fertility and increasing longevity mean that thisis increasing in almost all world regions; from 7% now to 10% by 2050 in high income countries(but to 13% in Japan); from 8% to 14% in China (16–17% in the Hong Kong and Macau specialadministrative regions); and from 9% to over 12% in India(42). Under the most pessimistic scenario,by 2050 the dependency ratio will have reached 20% in China(42).As the capacity of the informal care system is exceeded, current indirect costs are likely totranslate into increased direct costs. In high income countries, direct social care costs aregenerally subsidized to varying degrees and hence impose a significant cost burden on thenational exchequer. This, coupled with the high cost of residential care, accounts explicitly forthe focus in recent national dementia strategies to ‘invest to save’: reducing costs to governmentby investing in improved early diagnosis and caregiver support, hence delaying or preventinginstitutionalisation(8).Families worldwide need and deserve support, and for this the state is the ultimate guarantor.The WHO policy document ‘Towards an International Consensus on Policy for Long-Term Careof the Ageing’(43)describes principles to inform policies for sustainable programs in long-termcare that are consistent with the priorities of countries at different levels of development. Thereis wide variation between countries and cultures in the responsibilities of individuals, familiesand the state for long-term care. However, the WHO recommends that each community couldand should determine transparently the types and levels of assistance needed by older peopleand their caregivers, and the eligibility for and the financing of this long-term care(43). In practice,governments have not heeded this call, and relatively few, particularly in low and middle incomecountries, have comprehensive policies and plans(44).Studies from the 10/66 Dementia Research Group have highlighted the social vulnerability ofolder people with dementia in Latin America, India and China(45). Social protection is hard todefine, depending on an interaction between health status and dependence on the one hand,income sufficiency and secure living arrangements. In the Dominican Republic, rural Peru andMexico, rural China and in India, pension coverage was low and many people with dementia weresignificantly reliant on family cash transfers. Almost nobody with dementia reported receivingdisability benefits, even in countries where such schemes existed. In contrast with developedcountries, it is relatively unusual for people with dementia to live alone or just with their spouse;living with children or children-in-law is the norm, and three generation households (includingchildren under 16) are relatively common. Nevertheless, around one-fifth of people with dementia(10% to 37% by centre) were classified as having potentially vulnerable living circumstances (livingalone or with a spouse). In most places between 5% and 25% of people with dementia had nochildren available for support, because of infertility or migration.5 alzheimer’s disease international calls on governments worldwide to develop policies andplans for long-term care that anticipate and address social and demographic trends and havean explicit focus on supporting family caregivers and ensuring social protection of vulnerablepeople with dementia.Social pensions (universal non-contributory pension schemes) address these concerns directly,providing insurance against the risks that older people face, including uncertainty over how longthey will live, how long they will remain healthy, whether they can count upon the support of othersif they need it, and how long they can earn an income. Where they have been introduced, thesepensions have been shown to play a significant role in alleviating chronic poverty at householdand community level(46-48). Further, they serve to reinforce reciprocal family ties, changing the
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
47
perspective from one in which older people are seen as expending household resources to one inwhich they can be properly valued for their non-economic as well as their economic contributions.Dependent older people would be particularly likely to benefit – informal care would be bolsteredand paid care would be more affordable. There may also be a role for targeted disability pensionsand caregiver benefits, although eligibility testing would impose costs and potential bureaucraticdelays.6 alzheimer’s disease international supports helpage international’s call for governments tointroduce universal non-contributory social pension schemesi.7 alzheimer’s disease international calls on governments to ensure that people with dementiaare eligible to receive and do receive disability benefits, where such schemes are in operation.
helen Sr. has been experiencing moderate dementia for thepast ten years. She was a prolific artist, even through the earlystages of her dementia, until she lost her eyesight. her oilpaintings adorn the walls of helen Jr’s home as well as those ofmany family members, friends, and the people who purchasedher artwork at the many shows she participated in from the1960s through the 1980s. For the past three years helen Sr. hasbeen living at a small, private, residential group home for peoplewith dementia near Washington dC. her daughter, helen Jr.,and other family members live in the area and visit regularly.They feel that at Victoria house every person, from residents tofamily members and caregivers are ‘family’.
i http://www.helpage.org/Researchandpolicy/Socialprotection
Alzheimer’S diSeASe iNTerNATioNAl
48
World Alzheimer reporT 2010
references for conclusions And recommendAtions
1
Frytak JR, Henk HJ, Zhao Y, Bowman L, Flynn JA, NelsonM. Health service utilization among Alzheimer’s diseasepatients: evidence from managed care. AlzheimersDement 2008 September;4(5):361-7.Knapp, M. and Prince M. Dementia UK – A report into theprevalence and cost of dementia prepared by the PersonalSocial Services Research Unit (PSSRU) at the LondonSchool of Economics and the Institute of Psychiatry atKing’s College London, for the Alzheimer’s Society. THEFULL REPORT. London: The Alzheimer’s Society; 2007.Matthews FE, Dening T. Prevalence of dementia ininstitutional care. Lancet 2002 July;%20;360(9328):225-6.Macdonald A, Cooper B. Long-term care and dementiaservices: an impending crisis. Age Ageing 2007January;36(1):16-22.Canadian Study of Health and Ageing. Canadian studyof health and aging: study methods and prevalence ofdementia. CMAJ 1994 March 15;150(6):899-913.Llibre Rodriguez JJ, Ferri CP, Acosta D, Guerra M,Huang Y, Jacob KS et al. Prevalence of dementia in LatinAmerica, India, and China: a population-based cross-sectional survey. Lancet 2008 August 9;372(9637):464-74.Alzheimer’s Disease International. World Alzheimer Report2009. London: Alzheimer’s Disease International; 2009.Department of Health. Living well with dementia. ANational Dementia Strategy. London, UK: Department ofHealth; 2009.Dias A, Patel V. Closing the treatment gap for dementia inIndia. Indian Journal of Psychiatry 2009;51(5):93-7.
21 US Alzheimer’s Association. 2010 Alzheimer’sdisease facts and figures. Alzheimers Dement 2010March;6(2):158-94.22 Wimo, A., Johansson, L., and Jönsson, L.Demenssjukdomarnas samhällskostnader och antaletdementa i Sverige 2005 (The societal costs of dementiaand the number of demented in Sweden 2005) (inSwedish). Stockholm: Socialstyrelsen; 2007. Report No.:2007-123-32.23 Access Economics PTY Limited. The Dementia Epidemic:Economic Impact and positive solutions for Australia.Canberra: Access Economics PTY Limited; 2003.24 Alzheimer Society of Canada. Rising Tide: The Impact ofDementia on Canadian Society. A study commissioned bythe Alzheimer Society. Toronto, Ontario: Alzheimer Societyof Canada; 2010.25 Wimo A, Jönsson L, Winblad B. An estimate of theworldwide prevalence and direct costs of dementia in2003. Dement Geriatr Cogn Disord 2006;21(3):175-81.26 Ersek K, Kovacs A, Wimo A, Karpati K, Brodszky V,Jönsson L. Costs of dementia in Hungary. Journal ofNutrition, Health and Aging. In press 2010.27 Andlin-Sobocki P, Jönsson B, Wittchen HU, Olesen J.Cost of disorders of the brain in Europe. Eur J Neurol 2005June;12 Suppl 1:1-27.28 Allegri RF, Butman J, Arizaga RL, Machnicki G, SerranoC, Taragano FE et al. Economic impact of dementia indeveloping countries: an evaluation of costs of Alzheimer-type dementia in Argentina. Int Psychogeriatr 2007August;19(4):705-18.29 Zencir M, Kuzu N, Beser NG, Ergin A, Catak B, SahinerT. Cost of Alzheimer’s disease in a developing countrysetting. Int J Geriatr Psychiatry 2005 July;20(7):616-22.30 Wang G, Cheng Q, Zhang S, Bai L, Zeng J, Cui PJ et al.Economic impact of dementia in developing countries: anevaluation of Alzheimer-type dementia in Shanghai, China.J Alzheimers Dis 2008 September;15(1):109-15.31 Luengo-Fernandez, R., Leal, J., and Gray, A. Dementia2010. The prevalence, economic cost and researchfunding of dementia compared with other major diseases.A report produced by the Health Economics ResearchCentre, University of Oxford for the Alzheimer’s ResearchTrust. Cambridge: Alzheimer’s Research Trust; 2010.32 Goss, J. Projection of Australian health care expenditureby disease, 2003 to 2033. Canberra: Australian Institute ofHealth and Welfare; 2008.33 Australian Institute of Health and Welfare. Dementiain Australia. National data analysis and development.Canberra: Australian Institute of Health and Welfare; 2007.34 Shah A, Murthy S, Suh GK. Is mental health economicsimportant in geriatric psychiatry in developing countries?Int J Geriatr Psychiatry 2002 August;17(8):758-64.35 Wang H, Gao T, Wimo A, Yu X. Caregiver time and costof home care for Alzheimer’s disease: a clinic-basedobservational study in Beijing, China. Ageing Int. In press2010.36 Wimo A, Winblad B. Resource utilisation in dementia: RUDLite. Brain Aging 2003;3:48-59.37 Gustavsson A, Johansson L, Rapp T, Reynish E, OussetPJ, Andrieu S. Differences in resource use and costs ofdementia care between European countries: baseline datafrom the ICTUS study. J Nutr Health Aging. In press 2010.
2
34
5
6
78
9
10 Prince MJ, Acosta D, Castro-Costa E, Jackson J, Shaji KS.Packages of care for dementia in low- and middle-incomecountries. PLoS Med 2009 November;6(11):e1000176.11 Suh GH, Wimo A, Gauthier S, O’Connor D, Ikeda M,Homma A et al. International price comparisons ofAlzheimer’s drugs: a way to close the affordability gap. IntPsychogeriatr 2009 December;21(6):1116-26.12 Rafii MS, Aisen PS. Recent developments in Alzheimer’sdisease therapeutics. BMC Med 2009;7:7.13 Tout K. Ageing in Developing Countries. Oxford: OxfordUniversity Press; 1989.14 Prince M, Livingston G, Katona C. Mental health carefor the elderly in low-income countries: a health systemsapproach. World Psychiatry 2007 February;6(1):5-13.15 Arai Y. Japan’s new long-term care insurance. Lancet2001 May 26;357(9269):1713.16 Kikuchi K, Takahashi R, Sugihara Y, Inagi Y. Five-yearexperience with the long-term care insurance system inJapan. J Am Geriatr Soc 2006 June;54(6):1014-5.17 Kumamoto K, Arai Y, Zarit SH. Use of home care serviceseffectively reduces feelings of burden among familycaregivers of disabled elderly in Japan: preliminary results.Int J Geriatr Psychiatry 2006 February;21(2):163-70.18 Wimo A, Winblad B, Jönsson L. An estimate of the totalworldwide societal costs of dementia in 2005. Alzheimer’sand Dementia 2007;(3):81-91.19 Wimo A, Winblad B, Jönsson L. The worldwide societalcosts of dementia: Estimates for 2009. Alzheimers Dement2010 March;6(2):98-103.20 Wimo A, Jönsson L, Gustavsson A, McDaid D, Ersek K,Georges J. The economic impact of dementia in Europein 2008 – cost estimates from the Eurocode project.International Journal of Geriatric Psychiatry. In press 2010.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
49
38 Sousa RM, Ferri CP, Acosta D, Albanese E, GuerraM, Huang Y et al. Contribution of chronic diseases todisability in elderly people in countries with low and middleincomes: a 10/66 Dementia Research Group population-based survey. Lancet 2009 November 28;374(9704):1821-30.39 Sousa RM, Ferri CP, Acosta D, Guerra M, Huang Y,Ks J et al. The contribution of chronic diseases to theprevalence of dependence among older people in LatinAmerica, China and India: a 10/66 Dementia ResearchGroup population-based survey. BMC Geriatr 2010 August6;10(1):53.40 World Health Organization, Noncommunicable Diseasesand Mental Health. Innovative care for chronic conditions:building blocks for action: global report. Geneva: WorldHealth Organization; 2002. Report No.: WHO/MNC/CCH/02.01 – ISBN 92 4 159 017 3.41 Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH.Improving the quality of health care for chronic conditions.Qual Saf Health Care 2004 August;13(4):299-305.42 Harwood RH, Sayer AA, Hirschfeld M. Current and futureworldwide prevalence of dependency, its relationship tototal population, and dependency ratios. Bull World HealthOrgan 2004 April;82(4):251-8.43 World Health Organization. Towards an InternationalConsensus on Policy for Long-Term Care of the Ageing.Geneva: World Health Organization; 2000.44 Prince M, Livingston G, Katona C. Mental health carefor the elderly in low-income countries: a health systemsapproach. World Psychiatry 2007 February;6(1):5-13.45 Prince M.J. The 10/66 dementia research group – 10 yearson. Indian Journal of Psychiatry 2009;51:S8-S15.46 Garcez-Leme LE, Leme MD, Espino DV. Geriatrics inBrazil: a big country with big opportunities. J Am GeriatrSoc 2005 November;53(11):2018-22.47 Institute of Development and Policy Management/HelpAge International. Non-contributory pensions andpoverty prevention. A comparative study of Brazil andSouth Africa. London: Institute of Development and PolicyManagement; 2003. Report No.: Final Report, DFIDProject R7897, Pensions and Poverty Prevention.48 Gorman, M. Age and Security – How social pensions candeliver effective aid to poor older people and their families.Help Age International; 2004.
Alzheimer’S diSeASe iNTerNATioNAl
50
World Alzheimer reporT 2010
GlossaryADLBasic activities of daily living (ADL), such as eating,dressing, bathing, toileting, grooming, and gettingaround – sometimes referred to as personal care.CI / confidence intervalThe 95% confidence intervals give a range ofplausible values in the real world for what is beingobserved in the study sample, given the samplesize and the likely play of chance. This could be theprevalence or incidence of dementia, or an odds ratioor relative risk for an association between a risk factorand dementia. So, a prevalence of 6.0% with 95%confidence intervals of 4.5%-7.5% would mean that,given the likely imprecision of the estimate, the trueprevalence in the general population could be as lowas 4.5% or as high as 7.5%, but would be unlikelyto lie outside of these limits. A simple interpretationwould be that there would be a 95% probability thatthe true figure would lie somewhere between theseintervals.CoICost of illness. Cost of illness (CoI) studies aredescriptive. They can be used to quantify the totalsocietal economic burden of a health condition, andcan highlight the relative impact on different healthand social care sectors.ComorbidityThe presence of one or more disorders (or diseases)in addition to a primary disease or disorder, or theeffect of such additional disorders or diseases.HeterogeneityWhen summarizing findings across studies (whetherregarding the prevalence of dementia, or associationsbetween dementia and other factors) the results maybe similar (homogeneity) or different (heterogeneity).When the results are similar, this adds to ourconfidence. When different, this may be explained bya real difference in what one is measuring, or by thedifferent research methods used in different studies.HICHigh income countries. Based on its Gross NationalIncome (GNI) per capita, every economy is classifiedas low income, middle income (subdivided into lowermiddle and upper middle), or high income. Economiesare divided according to 2009 GNI per capitacalculated using the World Bank Atlas method. Thegroups are: low income, US$995 or less; lower middleincome, US$996 – US$3,945; upper middle income,US$3,946 – US$12,195; and high income, US$12,196or more.IADLInstrumental activities of daily living, such asshopping, preparing food, using transport, andmanaging personal finances.ImputationTo impute is to substitute an educated and informedestimate when a value is not available for an item ina set of data. For example, if no value for averagemedical costs was available for a country, that valuecould be imputed based on similar countries nearby.IncidenceIncidence is the rate at which new cases occur withina defined population. It is usually quoted in terms ofx cases per 100, per 1,000, or per 10,000 per year.The incidence of dementia increases exponentiallywith age, so age-specific rates are usually reported.Incidence rates can be used to calculate thenumbers of new cases over a given period.LMICLow and middle income countries. See also HIC.MorbidityMorbidity refers to the extent or distribution ofdisease within a population.MortalityMortality refers to the extent or distribution of deathswithin a population.PrevalencePrevalence is defined as the proportion of peoplein a defined population that has the disease at adefined time point or period. It is usually quoted asa percentage. In the field of dementia, prevalenceis often expressed as proportion of people withdementia in different age groups.
Alzheimer’S diSeASe iNTerNATioNAl
The GloBAl eCoNomiC impACT oF demeNTiA
51
Jody ross, a laughter yoga teacher in minneapolis, USA,visited lakeview ranch to lead a session with residents, staff,and a few visitors. elsie agreed to participate, but at first allher grimaces indicated that she knew she would not have agood time. Soon, however, she changed into an active andenthusiastic participant. The session ended with this hug.everyone was delighted and elsie and the other residents askedto have more such sessions.
Alzheimer’S diSeASe iNTerNATioNAl
52
World Alzheimer reporT 2010
Alzheimer’s disease internationalAlzheimer’s Disease International (ADI) is the international federation of Alzheimer associationsthroughout the world. Each of our 73 members is a non-profit Alzheimer association supportingpeople with dementia and their families.ADI’s vision is an improved quality of life for people with dementia and their families throughoutthe world. ADI aims to build and strengthen Alzheimer associations and raise awareness aboutdementia worldwide. Stronger Alzheimer associations are better able to meet the needs of peoplewith dementia and their carers.
What we do• Support the development and activities of our member associations around the world.• Encourage the creation of new Alzheimer associations in countries where there is noorganization.• Bring Alzheimer organizations together to share and learn from each other.• Raise public and political awareness of dementia.• Stimulate research into the prevalence and impact of Alzheimer’s disease and dementia aroundthe world.
Key activities• Raising global awareness through World Alzheimer’s Day™ (21 September every year).• Providing Alzheimer associations with training in running a non-profit organization through ourAlzheimer University programme.• Hosting an international conference where staff and volunteers from Alzheimer associationsmeet each other as well as medical and care professionals, researchers, people with dementiaand their carers.• Disseminating reliable and accurate information through our website and publications.• Supporting the 10/66 Dementia Research Group’s work on the prevalence and impact ofdementia in developing countries.ADI is based in London and is registered as a non-profit organization in the USA. ADI was foundedin 1984 and has been in official relations with the World Health Organization since 1996. You canfind out more about ADI at www.alz.co.uk.
Alzheimer’S diSeASe iNTerNATioNAl
muriel, in the foreground, has recently been diagnosed withearly onset Alzheimer’s. An emergency room nurse, shenow finds herself, at 58, the recipient of a different form ofcare delivery. muriel participates in a research and actionprogramme run by the Centre for memory resources andresearch (Cmrr) in Nice, France. here she is walking withNathalie, a psychologist, during an excursion to a local park.
alzheimer’s disease international:the international federationof alzheimer’s disease andRelated disorders societies, inc.is incorporated in illinois, usa,and is a 501(c)(3) not-for-profitorganization
alzheimer’s disease international64 Great suffolk streetLondon se1 0BLuKtel: +44 20 79810880fax: +44 20 79282357www.alz.co.uk